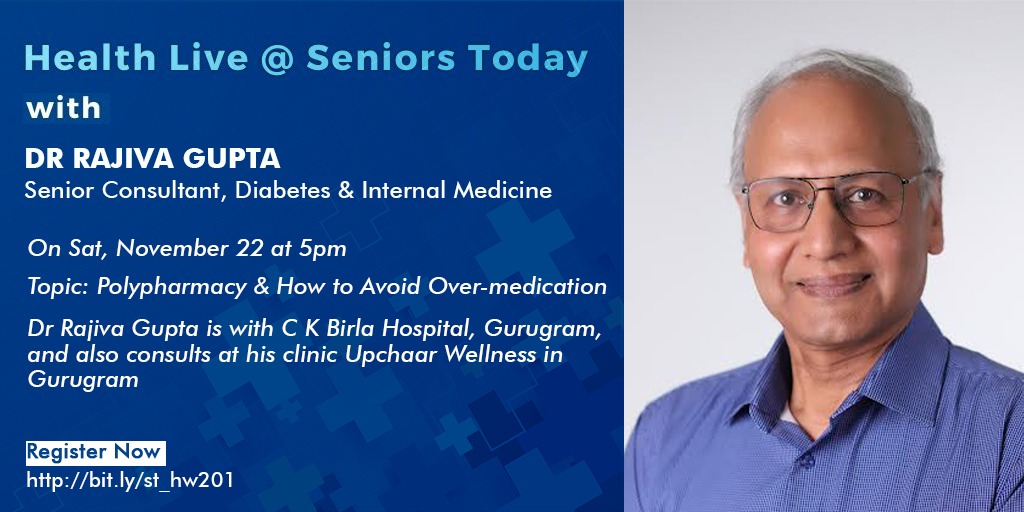
On 22 Nov, 2025, Seniors Today hosted their weekly Health Live Webinar with Senior Consultant, Dr Rajiva Gupta who spoke on and answered questions about Polypharmacy and How to Avoid Over- medication.
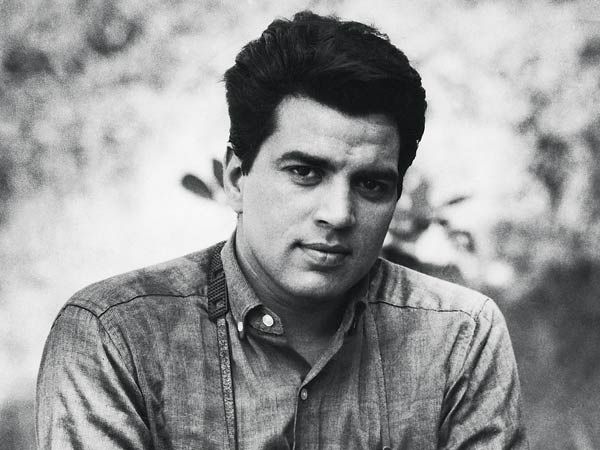
About Dr Rajiva Gupta:
Dr Rajiva Gupta is a Senior Consultant in Internal Medicine and Diabetes with an experience spanning over 40 years. He did his MBBS from Maulana Azad Medical College, New Delhi and MD from Dr. Ram Manohar Lohia Hospital, New Delhi (now called PGIMER – Post Graduate Institute of Medical Education & Research, University of Delhi). He has also done a Postgraduate Programme in Diabetology from the Johns Hopkins University School of Medicine, USA and a Specialist Certificate Course from the International School of Diabetes (IDF).
Dr Gupta currently has a consultation practice at his personal clinic Upchaar Wellness in Gurugram as well as affiliated with C K Birla Hospitals at Gurugram and Punjabi Bagh, Delhi.
He has been practising earlier at his clinic in Ashok Vihar Delhi and has been affiliated with major hospitals like Fortis Hospital, Shalimar Bagh, Max Super Speciality Hospital Shalimar Bagh, Delhi Heart and Lung Institute New Delhi etc.
Dr Gupta has conducted CME (continuing medical education) programmes in the fields of internal medicine with special focus on diabetes, clinical cardiology, and geriatrics and given lectures and conducted certified courses on various topics in diabetology, cardiology, critical care , geriatrics and Covid-19.
He has attended several national and international symposia, conferences and workshops under the auspices of leading organisations and institutions like Harvard University, American College of Cardiology, Cleveland Clinic, European Society of Hypertension , Indian Thyroid Society, American Diabetes Association, American Society of Hypertension etc.
Dr Rajiva Gupta has been an active researcher having participated in several national and global clinical trials in the fields of diabetes and cardiology. He is a member of several prestigious professional organisations like the Endocrine Society, American Diabetes Association, American Association of Clinical Endocrinologists, American College of Physicians, American College of Cardiology, Research Society for the Study of Diabetes in India , Geriatric Society of India etc. He has contributed articles in the fields of Vitamin D , Insulin therapy, Geriatrics in reputed journals.
Dr Rajiva Gupta has written a book “Stress & Diabetes: The Underappreciated Connection” published by the Pendown Press, New Delhi which was released at the New Delhi World Book Fair in 2023. He is also author of the book, Stress and Farigue | The Unnoticed Connection.
Two of Dr Gupta’s articles appeared as the Cover Story in the Seniors Today March 15 and November 15 issues. In March, the topic was Fatigue and in November, he wrote on Polypharmacy.
- Polypharmacy is a growing but often overlooked issue.
- Polypharmacy is defined as taking equal to or more than 5 medicines concurrently.
- The issue of polypharmacy has profound repercussions in seniors.
- With increasing longevity, chronic illnesses are rising. Managing multiple illnesses often leads to prescribing multiple medications.
- Polypharmacy has become extremely common in the elderly people.
- What starts as a well intentioned, well meaning treatment chart, turns into a medication overload with a potential to cause harm as well.
- Polypharmacy is called the hidden peril of modern medicine.
- In India, 1 in 3 seniors lives with polypharmacy.
- The burden is higher in the urban areas.
- 57% of seniors take more than 5 medications.
- More than 20% of seniors take more than 10 medications.
- 38% seniors are taking over the counter medication/ drugs.
- 63% seniors are taking herbal or alternative remedies.
– In the post hospitalisation phase, there is a surge in the medications prescribed.
- Usage of Polypharmacy has a profound impact.
- It contributes to 1/3rd of all hospital admissions.
- The risk multiplies with every pill.
- Studies show, with 2 medications the risk of adverse outcomes such as falls and hospitalisation rises to 13%. The risk increases to 58% with over five medications and 82% when the number of medicines increases beyond seven.
– Causes for Polypharmacy:
- Multi morbidity: this is defined as the patient having 2 or more medical conditions and each condition adds a treatment
- Multiple care givers
- Prescribing cascades: treating side effects as new disease
- Symptom overload: more the symptoms, more the drugs
- The expectation and request of the patient
- Over the counter supplements, vitamins, pills which are taken by the patient himself, since they are deemed to be harmless
- Self medication with antacids, blood thinners, sleeping aids silently keep aiding to the load of medications being taken
- It is not that medicines are bad. But with ageing the brain and body become more sensitive, therefore making the doses which are safe in the younger population can cause side effects in the seniors.
- Kidneys slow down as we age and the drugs stay in the body for longer due to the decreased filtration rate.
- Many drugs are metabolised in the liver. As we age, the liver function also reduces and the levels of sedative drug’s, blood thinners rise in the blood.
- As we age, there is muscle loss. There is more fat and less muscle thus fat soluble drugs accumulate. An example of such a drug is Vit D.
– Polypharmacy affects the health and everyday life of seniors in the following ways:
- Increased risk of falls, fractures, dizziness, decreased mobility and hospitalisation. The drug’s increasing this risk are sedative drugs, sedatives, certain blood pressure lowering medications
- Reduced appetite, energy and sleep
- Bowel and bladder effects
- Blood sugar fluctuations
- Polypharmacy affects memory, mood and attention
- Easy irritability, low mood
- Slow reflexes and increased reaction time
- Affects the daily life and increased dependence on family
- Drug interactions and drug induced illness. It can also cause a delay in diagnosis and treatment
- Drug interactions can cause harm. Such as taking an analgesic with a blood thinner can cause GI bleeding, taking an antianxiety medication with a sedative for sleep,can cause serious drowsiness and increase the risk of falls.
- Any new drowsiness, constipation, dry mouth, decrease in appetite, easy bruising or bleeding after starting a new medication should be treated carefully and as a possible side effect of the medication.