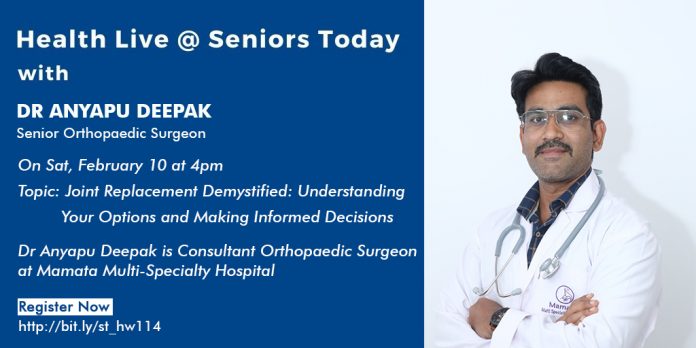
On 10 Feb, 2024, Seniors Today hosted their weekly Health Live Webinar with Dr Anyapu Deepak who spoke about Joint Replacement Demystified: Understanding Your Options and Making Informed Decisions and answered questions regarding the same.
Dr Anyapu Deepak is an experienced orthopedic surgeon equipped with a robust educational background, extensive hands-on experience, and a commitment to continuous learning and improvement. He holds an MBBS degree (Bachelor of Medicine, Bachelor of Surgery) from Guntur Medical College. He received his post graduation with an MS degree (Master of Surgery) in Orthopaedics from Rangaraya Medical College and a fellowship in Joint Replacement from Srikara Hospitals. He is currently working as a consultant orthopedic surgeon at Mamata Multi-specialty Hospital.
Osteoarthritis of the knee is not a disease, rather an inflammatory process instead of just simple wear and tear. Both the components contribute to osteoarthritis of the knee. Joint wear and tear along with the inflammatory process is responsible for osteoarthritis.
Because of inflammatory mediators, the synovial layer, cartilage- which are supposed to be smooth- gets degenerated due to inflammatory trauma which leads to roughness leading to pain on movement.
Osteoarthritis of the knee is the most common cause for pain and disability in the geriatric age group.
The most important symptom that brings the patient to the hospital is the pain.
Some of the patients might also have associated swelling (effusion) with the pain.
Some patients may also have a bony deformity.
Arthritis is not limited to only the knee joint, it can affect any joint. The knee joint being a weight bearing joint, it is most commonly involved.
Most of the paints that present with osteoarthritis of the knee, initially complain of pain localised to the inner side of the knee (lateral joint line), which can at a later stage progress to pain in the entire knee joint.
A study conducted in 2020 and 2022, says that sedentary lifestyle is more commonly seen in the big cities of the country, which is why the people staying in the urban population have a higher incidence of osteoarthritis of the knee, which is 33%
A higher incidence of OA knee is also seen in overweight and obese individuals.
A diagnosis for osteoarthritis of the knee is made with the help of an X ray.
Kellgren and Lawrence classification of osteoarthritis classifies osteoarthritis into 4 grades
Grade 1 and 2 is for mild OA
Grade 3 is moderate OA
Grade 4 is severe OA- this has severe loss of joint line, in raised osteophyte formation, subchondral sclerosis
Most of the Indian population falls under Grade 1 of the above mentioned classification where most patients are unaware of the disease. This is why education and awareness is necessary so the disease can be diagnosed at an earlier stage and its progress to grade 3 and 4 can be avoided or at least delayed.
Risk factors include:
– Females > Males
– Sedentary lifestyle
– Obese/ overweight patients
Treatment modalities and management includes the following:
1. Topical NSAIDs
2. Oral NSAIDs
3. Supervised exercises
4. Weight reduction and a healthy lifestyle
5. Patient education
If the patient after receiving the above mentioned conservation management continues to have persistent pain and symptoms, then we move to the next line of management which includes:
1. Intra articular injections- steroid injections- these are quick acting but short lasting, viscosupplements and PRP injections- are slow acting but long lasting— this means that these injections are an adjuvant to treatment and not the mainstay of treatment
If the symptoms still persist, then you have to look into the option of surgical management. These include:
1. Osteotomy- to correct the axis of the knee joint
2. Unicompartmental knee arthroplasty- done in patients with only inner side knee pain, the outer side of the knee should be completely pain free. This is preferred to some patients over total knee replacement because this surgery results in less blood loss, faster recovery and quicker rehabilitation.
3. Total knee replacement- this surgery has come a long way with respect to the technique, the implants, etc.
All the available implants give a life of 20-30 years, and it is bet if your treating physician decides which works best for you.
However, the most common complaint following a TKR (Total Knee Replacement) Surgery is the unmet expectation of the patient.
Other minor surgical complications include:
– Joint stiffness
– Inflammation
– Paresthesia
– Infection
The most common major surgical complications include:
– Readmission for re surgery
The prevalence of these complications is very low compared to the number of surgeries being performed.
The decision of whether a patient should undergo a Total Knee Replacement Surgery is not just based on the X ray of the patient but the X Ray is also correlated to the symptoms of the patient and this clinical presentation and examination and clinical findings.
Post operatively, you will have pain, but you need to compare it to the pain you had pre operatively and know that with time and rehabilitation knee exercises, it will get better.
The swelling and pain takes about 1-2 weeks to subside and then it gradually starts subsiding.
If you get single knee joint replacement surgery, it takes about 1 day, the day following your surgery, as your pain allows, you can start walking with the help of an aid.
You will require aided physiotherapy for 2-3 weeks following the surgery, after which you can continue on your own.
Your expectations following the surgery should be realistic. Yes, you can squat and sit cross legged but it is not advised to do so on the regular. However, occasionally, yes you can.
Most common cause for patient dissatisfaction is residual pain- 100% of pain relief cannot be assured.