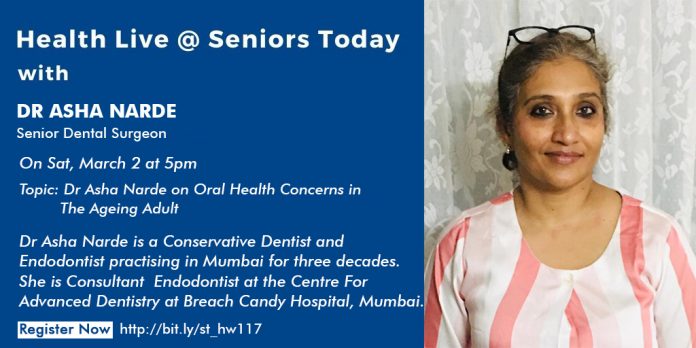
On 02 Mar 2024, Seniors Today hosted their weekly Health Live Webinar with Dr Asha Narde, a Senior Dental Surgeon who spoke on and answered questions about Oral (Dental) Health concerns in Ageing Adults.
About Dr Asha Narde:
Dr Asha Narde, a Conservative Dentist and Endodontist, has been in clinical practice at Juhu, Mumbai since 1995. She graduated from Nair Hospital Dental College in 1990 and subsequently did her post graduation from the KLES Dental College, Belgaum, in 1994. Dr Asha Narde is a Consulting Endodontist at The Centre For Advanced Dentistry, Breach Candy Hospital and for the past 16 years has been working alongside Dr Rajeev Narvekar in South Mumbai.
A great majority of her patients are 60 years and above, and providing optimum dental care has been her mission. She is part of the fraternity that trains young dentists in the field of geriatric dentistry to understand and provide the needs of the ageing population in an objective manner.
50% of the patients above the age of 60 years are medically compromised, and are on medication for:
- Diabetes mellitus and related complications
- Hypertension
- Cardiovascular Disease
- Arthritis
- Cancer
- Degenerative Neurologic and neuromuscular disorders like Muscle Atrophy, Alzheimer’s, Parkinson’s, and Myasthenia Graves
- Chronic obstructive pulmonary diseases
- Gastric Problems
Of this 50%, 27% of elderly have more than one comorbidity
24% of this population has difficulty performing their daily functions such as walking, eating, visiting the toilet, etc.
40% have a disability of some sort
20% of the elderly suffer from mental illnesses.
In the midst of all of this, it is important that a healthy dentition is maintained by all adults.
The World Social Report 2023 states that there should be no-one left behind in the aging population and everybody’s general and oral health should be taken care of. Guidelines have been put in place to ensure the same.
Importance of maintaining a naturally healthy dentition has been stressed upon, from the structural, functional and psycho-social point of view.
The number of teeth present in the mouth is a predictor of mortality, irrespective of the socioeconomic status and lifestyle. Increased longevity is believed to be dependent on the increased number of teeth.
Adequate nutrition promotes health and a sense of well being in ageing adults. Inadequate nutrition may contribute to an accelerated physical and mental degeneration. Oral health and general health are closely linked. Disorders of the oral cavity contribute to poor eating habits which in turn can be detrimental to the nutritional status and general health of the individual.
Loose, painful teeth, ill fitted dentures, oral lesions, dry mouth may result in a reduced desire and inability to eat leading to lean body mass and lower exercise levels. This can also further lead to iron, calcium and other supplemental deficiencies leading to anemia and osteoporosis.
Chewing activity is beneficial for cognitive functions. Chewing activity produces a rhythmic movement which improves the blood flow to the brain cortex, this helps in maintaining the cognitive function of the brain.
Natural teeth support crowns, bridges, over dentures and removable dentures. Natural teeth help maintain the function of proprioception.
Poor oral appearance and bad breath can impede social interaction
Some common dental problems include:
- As age progresses, the chewing surfaces of the molars tend to flatten resulting in lodging of food leading to cavities.
- Plaque accumulation can occasionally lead to secondary caries.
- Dry mouth with mucosa ulcerated, cracked lips, and fissured tongue. Polypharmacy is a common cause for dryness of mouth.
- Increase in cavities especially around the roots.
- Wearing of the teeth- when it is one the chewing surface it is called attrition, when it involves the sides of the teeth it is called erosion.
- Deterioration of gum health (looseness of teeth), inflammation of gums, and gum recession.
- Lack of dexterity due to advancing age can affect how oral hygiene is maintained.
Every adult should visit their dentist at least once every 6 months.
When you visit your dentist regularly, it is easier for the dentist to point out the problem and treat it at an earlier stage.
You can also use fluoride toothpaste.
You can also use remineralising pastes such as chlorhexidine 0.12%, 1% or 2% gel / varnish to reduce bacterial concentration and risk of caries as advised by your dentist. This helps strengthen the enamel.
Salivary substitutes are available to improve hydration, lubrication and self cleaning in individuals with a dry mouth.
Occasionally, if the cavity is more severe, restorative procedures can be done. These procedures revolve around preserving dental tissues with minimally invasive techniques using cariostatic, bioactive and fluorinated fillers in the restorative matrix.
Xerostomia:
It affects 30% of patients older than 65 years of age and upto 40% of patients older than 80 years.
Cause:
- Polypharmacy
- Comorbid conditions like diabetes, Alzheimer’s disease, Parkinson’s disease
Signs and symptoms:
- Mucositis
- Caries
- Cracked lips
- Fissured tongue
Recommendations:
– Plenty of oral fluids during the day
– Limiting alcoholic beverages, beverages high in sugar or caffeine, juices, sodas, teas or coffee.
Associated risk factors:
- Root caries
- Secondary Coronal Caries
Available treatment options:
– Adopting good oral hygiene
– Use of rotating / oscillating toothbrushes
– Use of topical fluoride (mouth rinses, toothpaste and varnish)
- Use of silver diamine fluoride to prevent and arrest root caries
Radiation caries:
Radiotherapy is often used as a palliative treatment for malignancies. Patients with Head and Neck Cancer (HNC) are usually subjected to high doses of radiation where maxilla mandible and salivary glands are exposed. This can result in radiation caries which is a late indirect effect of radiation therapy.
Commonly affected sites are the cervical and incisal edges of the teeth, it can also rapidly involve the pulp.
Side Effects:
- Alteration of the crystalline structure of enamel
- Weakening of dentino-enamel junction
- Damage to intra and intertubular collagen
- Fall in the Salivary pH falls from 7 to 5
Any dental treatment should be completed before starting the radiation therapy. Teeth with severe pulpal/periodontal infection should be extracted pre-radiation
A dental prophylaxis with fluoride application should be performed.
Instructions for rigorous oral hygiene measures should be told to the patient
Use of salivary substitutes in case of drv mouth is advised.
Endodontic therapy in patients on bisphosphonates:
High dose bisphosphonates are prescribed to patients undergoing treatment for breast cancer, prostate cancer or multiple myeloma with bone metastasis.
This needs to be disclosed to your treating dentist.
These agents depress osteoclasts and diminish resorption of bone. And can lead to a high risk for necrosis of the jaw.
General dental care habits should include:
- 6 monthly, periodic visits to your dentist
- Maintain a good oral hygiene
- Brushing your teeth twice daily
- Use a fluoridated toothpaaste/ desensitising toothpaste or remineralising applications
- Use of mouthwash, flossing and interdental brushes
- Use of a water flosser is also advised
- Drink plenty of water
- Maintain a well balanced and nutritious diet