Vinita Alvares Fernandes narrates her experience of undergoing a stent angioplasty
Rewind to thirty or forty years ago — I often wondered why a doctor would ask for your family medical history on your first visit? Especially when you have tonsillitis and you are eighteen years old.
I now realize family history plays an all-important role for the early detection of diseases. When those early signs of disease do not show up or you brush them aside with positive thoughts or the feeling that you are invincible, I say this today — know how important it is to take these signs very seriously.
Here’s my personal experience —
From the time I was asked to do an annual medical checkup for my first job and annually subsequently, (here in India we do take medical checkups for granted, often stretching them to once every two to three years unless mandatory) I maintained a pretty balanced lifestyle of daily exercise, eating fruit, nuts and raw vegetables, cutting back on fried food and processed stuff. No alcohol, no smoking (passive smoking can’t be helped) no social drugs, except for desserts in abundance, I thought I was doing pretty well for myself, only to realize that genetics and hereditary are a complicated matter and can hit you with any disease at anytime, often catching you unaware. Disease stemming from family history should always be at the back of your mind, this is something you need to live with, grow with and address as you live. Coming from a family history of heart disease from my paternal side and thyroid issues from my maternal side, I should have learnt from my pregnancies when high blood pressure and gestational diabetes hit me that I needed to thread with caution and that daily exercise and a few healthy option foods would not cut it. I did take good health for granted, not having any major health issue since the birth of my children, twenty-three years of good health, kind of gave me the vision that I was on the right track.
I belong to the nature cure, ‘food is medicine’ brigade, so when I was asked to start a statin a few years ago, because of family history, I slyly declined the doctor’s advice and continued to live by nature cure. All signs of chest tightness were attributed to stress and anxiety as I never felt tiredness or breathlessness and walked my ten to twelve thousand steps plus one hour of Iyengar yoga six days a week.
THE FIRST SIGN — One day I experienced a giddy spell after my yoga class and on taking my blood pressure, saw it was unusually high, this settled in a few days naturally. The chest pain and slight heaviness in my head continued.
What exactly did I feel?
Like you want to burp and the burp is not released, like air bubbles are trapped in your chest and intestines, sometimes you can’t take a deep full breath but normal breathing is fine, occasional pain in shoots or stings in your chest area and your neck and shoulder area feels stiff. All this passed and life was well again.
I also believe that I am divinely protected, good or bad, foolish or wise I don’t know, but I tend to live life fearlessly with this belief. Here’s how my story unfolds with divine protection leading me to safety.
THE SECOND SIGN— A deep tissue massage, led to soreness of my left shoulder blade, this slight swelling but acute soreness, burning sensation and shooting pain at times for over two months permeating to the chest led me to investigate. A visit to the Physiotherapist confirmed a muscle spasm and a 2D-echo confirmed all was well with my heart.
The marvel of a curious doctor, suggested (not on an urgent basis) a CT angiogram to rule out all doubts, given my family history, yes here is where the family history came into play again.
It was this CT angiogram that revealed a little something that was in hiding for who knows how long.
The report suggested an angiogram and one knows that an angiogram is almost always followed by an Angioplasty; it’s just a matter of how many tubes need cleaning. Hmmm, sounds so clinical but it is the very truth. Exactly the way it panned out for me.
The three important parameters to clear—
ECG
2D Echo
CT angiogram
if these are clear you are home safe.
Once the CT angiogram reported irregularities, there was no time to be wasted.
I was asked to do a few tests — CBC, Creatinine and of course RCPTR, admitted early next morning and before I could catch my breath, I was on a stretcher being wheeled into the Cath Lab.
How Do You Prepare Yourself Before You Get Admitted —
Physically
remove all body hair
good clearing of the bowel
put together a mini toilet kit
your medicine pouch
your medical file
no lenses, no false teeth
a set of clothes
disposable slippers
eye mask
ear plugs
phone – ear phones-charger (optional)
Emotionally
keep the deep breathing exercises going
happy thoughts that ‘this too shall pass’
force a smile, it automatically relaxes the body
carry some inspirational reading
if you have your phone, nothing like music to soothe the soul.
What is an Angiogram?
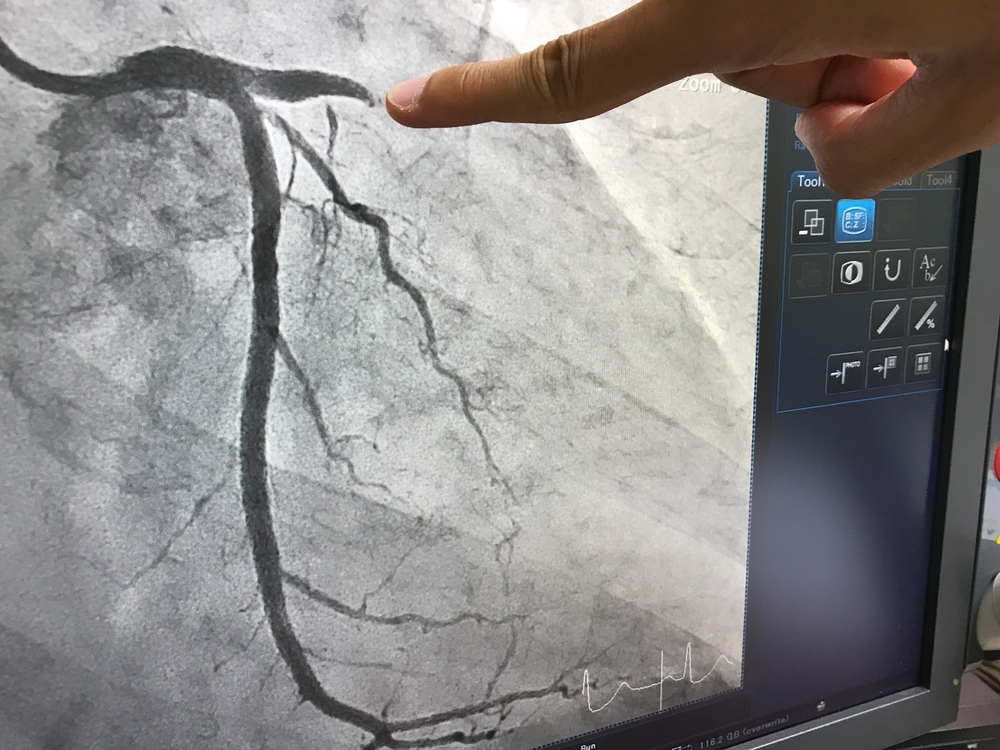
An angiogram is the injecting of a contrast dye into the coronary artery to identify blockages caused by plaque by taking X-rays, pictures of the heart from various angles.
The entire procedure from start to finish takes about fifteen minutes.
You will be wheeled in on a stretcher and transferred to the X-ray table and hooked up to a heart monitor, and an intravenous (IV) infusion set on one arm, the butterfly IV needle, a device used to gain access to the vein to draw or inject multiple medication through one access point. Here you will have the glucose drip, painkillers or sedation injected through the (butterfly) winged infusion set.
They then prepare two or three sites as access points to the arteries by sterilization and numbing of the sites, (usually the other arms wrist and both thighs) it feels like a mix of cold, a little burning cum stinging sensation for just a few seconds and finally tape your arm down to immobilize it for the procedure. (mine was done through the arm) Once you are hooked up, your stretcher is adjusted for the camera and you are all set.
TIPS
-Tell the nurse if your veins are fine before inserting the intravenous (IV) infusion set, make sure it is taped to the wrist name band (less tape on the skin the better) this way it cannot be pulled or tugged accidentally.
-When moving from one stretcher to the other, bend your knees, put pressure on your feet and lift your butt, it will help the staff slide you with ease.
-Lay your arms flat beside you in a comfortable position, they will stay in this locked position for a couple of hours, leave a gap between your arm and armpit and rest your wrist on the table. It is very important to take time to position yourself comfortably before they tape your arms down. A locked shoulder is unnecessary added pain, that too excruciating pain.
The anesthetist will introduce herself and tell you what to expect and the cardiac surgeon will tell you what to expect too.
So you will be aware of all the hustle and bustle around you, the moving of the X-ray machine above you, and the odours of hospital solutions and the professionals chatting. You have the option of just shutting your eyes, and zoning into a meditative state of mind, put a smile on your face, it actually reduces the tension, say a prayer not for yourself but for the doctor, the medical staff around you that they may act in unison for the procedure, with precision and perfection. Frankly, it’s really not your business to be part of the nitty gritties of the procedure, so don’t add to your stress and zone out is my fervent request, especially for the faint hearted. This is the best advice I could give you.
Let the doctors take charge
Once the prep is complete, each member of the team calls out ‘Ready’ to make sure all are on the same page.
You will be sedated, the anesthetist at this point will numb the area and begin the inserting of a thin tube catheter and straw, you will feel some mild discomfort as a balloon is inflated to stretch the artery and a little bit of medication injected, to keep the artery from clamping down when injecting the contrast.
The TV monitor directs the surgeon to get the catheter to reach right into the heart, then the fluid (contrast dye) is inserted to show up clearly on the X-ray
monitor where and how the blood is flowing in the arteries, and all parameters are viewed and photos of the arteries of the heart at different angles are taken.
Your doctor will then command you to take a deep breath, hold it, till he asks you to release, and breathe normally.
This happens twice.
Angiogram done!
Once the angiogram is done, the pictures are closely viewed and the decision of minor blockages, major blockages, angioplasty to insert stents or a bypass are made on the spot, reported to next of kin for approval and onward to the next step.
Why it is a better option to go through the arm versus the groin for the procedure?
There are two methods of conducting an angioplasty through the artery in the wrist or through the groin. If you are given the choice, always opt for the arm, the healing, recovery, pain and mobility is easier to deal with post procedure in every which way.
ANGIOPLASTY
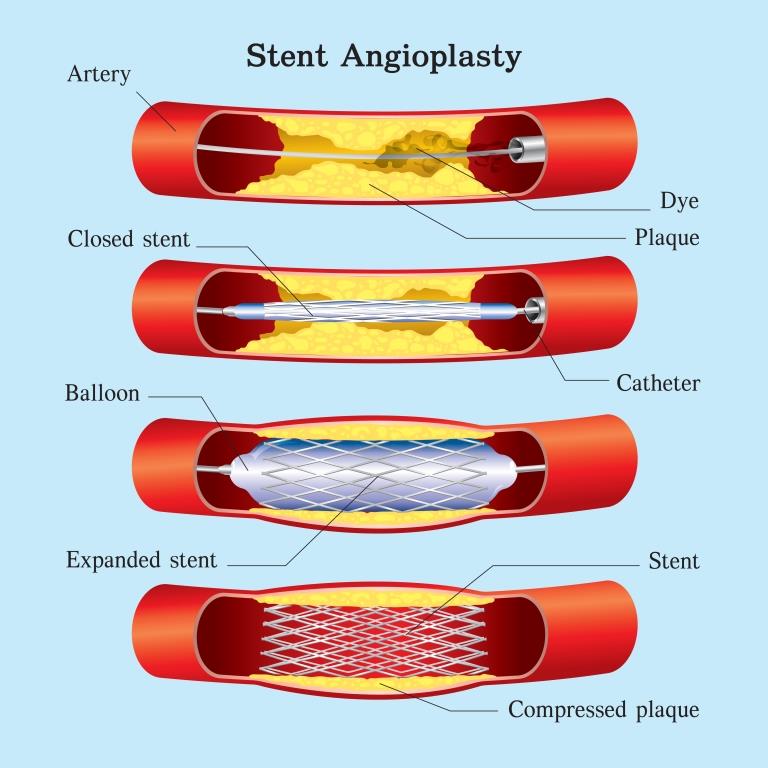
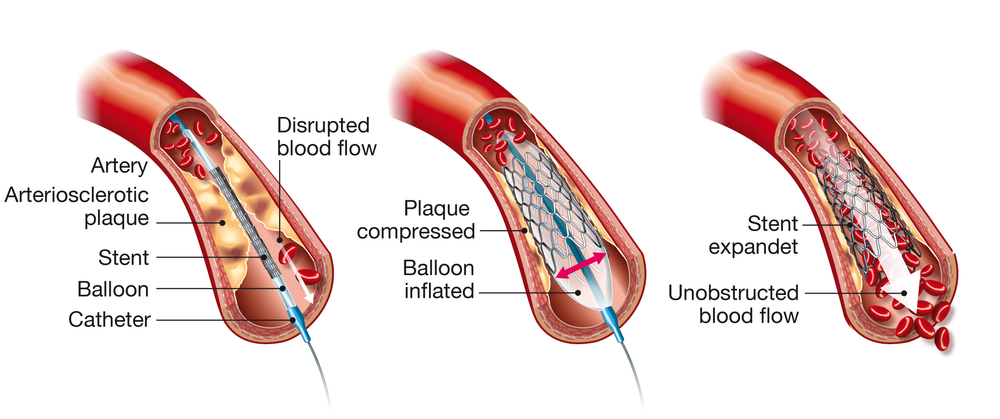
The steps that involve an angioplasty are —
Placement of the catheter
Inflation of balloon to open blocked artery
Inserting stent
Removal of catheter
If it is immediately followed by an angiogram, the first two steps are already in place, which makes the procedure half the duration.
The procedure is usually done under sedation and local anesthesia.
It can take between thirty minutes to two hours.
The catheter is inserted in the artery and a tiny wire is threaded to the blocked artery with the help of X-ray imaging. This serves as a guide for the balloon catheter.
The balloon catheter presses the plaque against the artery wall and opens the blockage for inserting the stent. (A tiny tube made of fine wire mesh, which keeps the artery open)
The stent once fixed to the artery wall usually does not ever move.
Once the green signal is on —‘ready’ all concentration is on the surgeon. A puncture in the wrist and inserting of catheter is already in place; a six-inch needle is gently pierced into your artery, for which you will only feel a slight prick.
REMEMBER—do not look at anything that is going on, surrendering to the unknown is the best way out.
The sharp, loud crystal clear commands of the surgeon, will give you a feeling of calm and confidence.
‘Ready’
‘Let’s start’
‘Show me down’
‘That’s excellent’
‘What is your name?’
‘Akash’
‘Nobody has shown me down this perfectly, I am pleased with you.’
(the showing of the heart from different angles)
‘Give four tablets’
‘Vinita start crunching on the tablets, crunch, crunch and swallow, good’ (sedation medication)
‘Now give three more, crunch, sip more water, swallow, excellent’
‘We are sedating you, you will not feel a thing, just close your eyes, you need to do nothing, it will be over soon.’
(All of this I hear in the background while I keep my eyes shut)
‘Ready for shoot, move I c, 11,12,13,14, go up, ready for shoot’
‘Ready sir’
‘Ready sir’
‘Shoot’
‘Excellent’
‘Now do you see this, it’s a bend, no problem, the wire will find its way, a little difficult, but it’s ok, let’s go’
‘Go to 14-15-16’
‘Ready for shoot’
‘Ready sir’
‘Ready sir’
‘Shoot’
‘Do you see how it found the way, it’s all good.’
‘Almost done, check, show 1C, move left, up, a bit down’
‘All clear’
‘Done.’
‘Ok Vinita, all done, all successful, they will now remove the catheter, stay still, you will feel a pulling sensation, just take deep breaths and relax.’
This is the only part that caused pain, as they pull out the catheter, centimeter by centimeter you feel a pulling sensation it has to be done really slowly with multiple breaks to prevent the artery from going into a spasm, though it takes no more than two minutes in all, it feels like eternity.
‘Four centimeters to go, now three, two and it’s done.’
The incision is padded and taped,
‘Keep your arm bent and lay it on your chest for the next couple of hours.’
Within a few minutes you are on your way to a new environment of friendly smiling nurses welcoming you to the ICU to be hooked up 24/7 to monitors.
Remember— you can change the monitor cap from finger to finger, hand to hand to feel comfortable.
If there is one thing hospital ICUs’ don’t let you do, it’s sleep, always carry along an eye mask and ear plugs for some shut eye as day or night the activity level is continuous and loud with bright lighting.
You are usually the only patient eating meals in the ICU, the portions and courses are way too much, divide it into three meals and ask for it to be saved in the pantry, know that if you are hungry between meal times, it takes forever and ever to get a morsel of food at the wrong time.
You don’t need to guzzle water to flush your kidneys of the dye used for the procedure, half a glass of water every hour to cover two liters in a day is fine, this way you have bladder control and don’t need to keep asking for the bottle or commode seat.
In twenty-four hours you are discharged.
‘Prepare for discharge,’ the minute the nurses hear that, they buzz faster than ever, making sure the checklist is covered.
‘Make your going home outfit special,’ I say, leave the hospital looking snazzy, it feels so good. Even the staff feels good to let you go, as the stand in a single file at the entrance as your wheelchair passes through the door and you wave and say thank you and good bye. I always gift the staff a cake, after all doctors and medical staff always see you at your worst and rarely at your best, it’s a profession of self-sacrifice, all honour for those who embark on the journey to save and better the health of humans.
The Recovery Period—
This is the most important time for your body, when you are in recovery is the time your body tells you how brave you have been through the procedure but the truth is that you have taken an overall beating and it has to adjust to the medication and the procedure it has undergone. The effects of this beating now manifests in all kinds of unexpected ways. The good news is that the doctor always has a solution, one more prick or one more tablet often added to the list.
– You will feel different kinds and levels of pains.
– You will feel sensitive to every touch.
– You will feel cold due to weakness, rub your palms to generate heat, it improves circulation.
– Your mind automatically addresses the most painful part at a time.
– You will feel overall stiffness of the body, keep changing your sleep and lying down positions at least every two hours, slowly.
– Eat six to eight fist size meals every three hours; this will keep your metabolism up in your sedentary state. It’s good for your blood sugar and your digestive system. Sit upright when eating reading using the phone, not slouched in bed.
– Keeping yourself hydrated is another very important aspect of recovery, two liters of water and one liter of other liquids is the norm.
– Your body needs getting used to a whole new set of medicines, and you need to now administer them to yourself, timely. Make a list of medication to be taken at breakfast, lunch, dinner; do not rely on your memory.
– Icing the inflamed spots continuously is imperative; use ice packs as often as possible for long periods of time throughout the day, till all bruises disappear totally, even if the pain completely subsides.
– Your daily hygiene routine becomes more and more possible to handle on your own and within a week of the procedure your arm can maneuver itself almost as before.
– Aspirin can cause a lot of acidity and indigestion, take it after a heavy meal, I read somewhere that it’s better to take it at night as most heart attacks occur early morning a the effect of the aspirin is still strong twelve hours later rather than twenty plus hours later.
– It takes two to three weeks for you to regain physical strength and the spirit to get back to chatting with family and friends, short outings in small groups, slow walks all begin to take shape.
My mum always told us, nothing makes you feel better than dressing up and showing up, look in the mirror, smile for the new day of renewed strength.
‘This too shall pass’— it always passes.
– Doctors’ visits at the two-week and one month mark should take place. Keep your list of queries ready and daily readings of your blood pressure, oxygen levels and blood sugar if needed.

– Walk five minutes and build to fifteen two to three times a day at week two gradually increasing to half hour by week four. Walk on an empty stomach; heart patients need to do the reverse, not right after meals but one hour after a meal. While walking clasp your hands with straight arms at the back, you can take support of your butt, this stretches and strengthens the trapeze muscles.
Remember the heart is a muscle; it needs to be stretched all the time to stay healthy.
– Watch happy movies, it will relax you.
Welcome to your new life, there is no turning back from a lifestyle of heart healthy foods, exercise and happy living.
You are now twenty years younger in your heart.