On 30 Nov, 2024, Seniors Today hosted their weekly Health Live Webinar with a Senior Gastroenterologist, Dr Prasanna Shah who spoke on and answered questions about Crohn’s Disease and Inflammatory Bowel Disease.
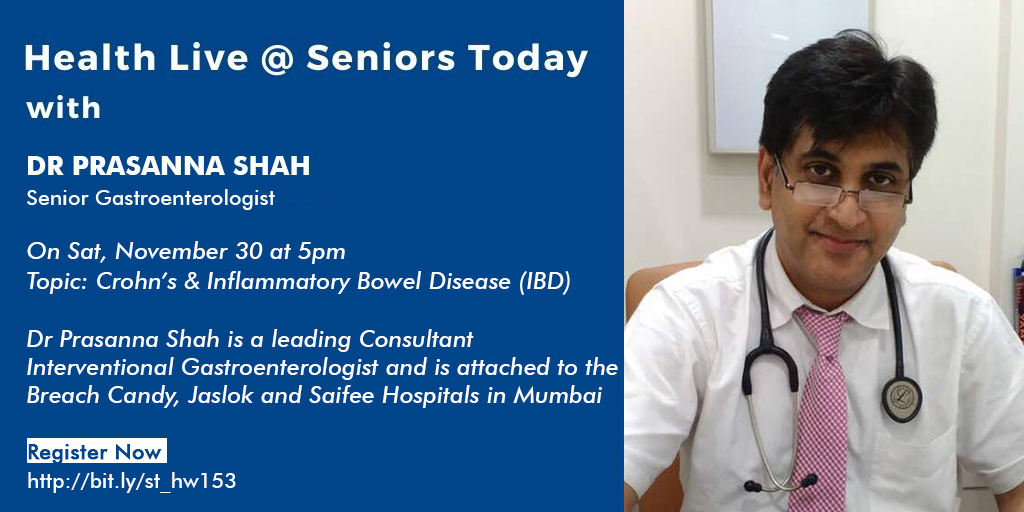
About Dr Prasanna Shah:
Dr Prasanna Shah is a leading Consultant Interventional Gastroenterologist and is attached to the Breach Candy, Jaslok and Saifee Hospitals in Mumbai. He has vast experience in therapeutic endoscopy and now metabolic correction endoscopy for weight loss.
Inflammatory bowel disease (IBD) is a complex and debilitating disease.
Inflammatory bowel disease has 2 components:
- Ulcerative colitis
- Crohn’s disease
There are very subtle changes between the two.
The main line of treatment and certain dietary do’s and don’t’s are fairly the same both the diseases.
The difference between ulcerative colitis and Crohn’s disease is that in Crohn’s disease one can get fistulas, peri anal abscesses. Whereas in ulcerative colitis, these are uncommon.
Inflammatory bowel disease has been there for a very long time. In the early 80s- 90s it was thought that Crohn’s is never seen in India, but it has always been around. But it’s now that the incidence is increasing and we’ve started recognising it.
There has been a rise in the number of cases of inflammatory bowel disease in the past 5 years.
Inflammatory bowel disease affects both the age groups- it has a bimodal presentation i.e. it can affect individuals in their teens to adulthood (15 to 30 years of age) and it can also affect individuals over the age of 60.
Inflammatory bowel disease is a long term/ chronic disease.
Inflammatory bowel disease in only very very rare cases leads to death.
Investigations done for Inflammatory bowel disease:
- Blood investigations which include CBC, ESR, C reactive protein
- ASCA (Anti Saccharomyces cerevisiae antibodies)- however this investigation is not very sensitive or specific
- Stool examination including stool routine and microscopic examination, stool fecal calprotectin, stool for occult blood
- CT abdomen, pelvis- Crohn’s disease as opposed to ulcerative colitis can present as a stricture. If necessary, CT scan of the small and large intestines may also be done- in Crohn’s disease the small intestine is affected. In ulcerative colitis, both the large and small intestine is affected.
- MRI- to get more information about the extent and degree of inflammation, character of the stricture, etc.
- Capsule endoscopy- ensure that no stricture is present. We see small ulcerations with normal intervening mucosa. In a patient with ulcerative colitis there is no intervening normal mucosa. There is extensive ulceration seen with friable mucosa. In Crohn’s disease we also get to see aphthous ulcers with normal intervening mucosa.
- Colonoscopy followed by biopsy
- Small bowel enteroscopy followed by biopsy
In Crohn’s disease the rectum is not affected. In ulcerative colitis, the rectum is affected all the way up.
Dr Shah urges the audience to refrain from reading about the disease on the internet. He emphasises on the fact that your doctor, dietician and nutritionist is the best guide.
Management modalities:
- Pharmacological- it includes immunosuppressive drugs, ASA compounds
- Good nutrition
- Biosimilars
In very severe cases with strictures, the patient might have to undergo surgery. But there has been a lot of advancement in the field of medicine since. And so now we have better options for treatment and management.
Lifestyle changes are an important aspect in the treatment of inflammatory bowel disease because stress and stressors are known to flare the disease.