“Ageing is an issue of mind over matter. If you don’t mind it doesn’t matter.” —Mark Twain
The humour in this quote sidesteps the grim reality of the ravages of ageing on the cardiovascular system.
Senescence stealthily slithers up on each and every one of us. It is unavoidable, but with careful monitoring it is possible to recognise, minimise and sometimes treat its effect on the cardiovascular system.
Senescence affects the blood vessels, the heart muscle, some heart valves and the electricity generating and conduction system of the heart.
Ageing of the Blood Vessels:
As a consequence of Ageing there is loss of Elasticity of the blood vessel wall in large and medium sized arteries. This causes a rise in the systolic BP which in turn causes further damage to the blood vessel, impairs organ blood flow and forces the heart muscle to do more work causing an inordinate strain. It must be emphasised that there may be no symptoms to alert an individual to this process and hence occasional measurement of BP is advisable to nip the problem in the bud.

The BP should be periodically checked using a digital home apparatus. The BP should be less than 140/90 mm Hg for any senior citizen. If higher, medical advice and treatment should be sought. Maintaining a normal BP will considerably reduce the risk of strokes, heart attacks and heart and kidney failure.
It is necessary to check for Diabetes. The best diagnostic test is a Glycosylated Hemoglobin (HbA1c) level in the blood. It is an accurate estimate of the average blood sugar over the preceding 3 months. Its level should be 6.5% or less. If higher then treatment is necessary starting with life style modifications of diet and exercise, drugs like SGLT2 inhibitors , Metformin and other medicines will be prescribed as required. It is recommended that every diabetic patient should take an SCLT2 inhibitor, if not contraindicated, as these drugs offer very significant protection to the heart, kidneys and the brain.
A close watch should also be kept on the Lipid Profile. The Total Cholesterol should be around 150 mg%, the LDL or “bad” cholesterol should be around 100 mg%, the HDL “good” cholesterol should be more than 45 mg% and the Triglycerides below 150 mg%. These levels are for those seniors without established CVS disease. Those with disease need still tighter control with LDLC levels as low as 55 mg%.
These levels can only be achieved with a combination of diet, exercise and Statins.
There are many misgivings about the side effects of statins. Suffice it to say that Statins are “life savers”, as they not only reduce cholesterol to target levels but also have a host of salutary effects on the blood vessel wall. They undoubtedly reduce heart attacks and strokes and every senior should take a statin if he has CVS disease.
Close attention to BP, Blood Sugar (Diabetes) and Lipids will go a long way in slowing down the ravages of senescence.

Ageing and malfunction of the Heart Muscle:
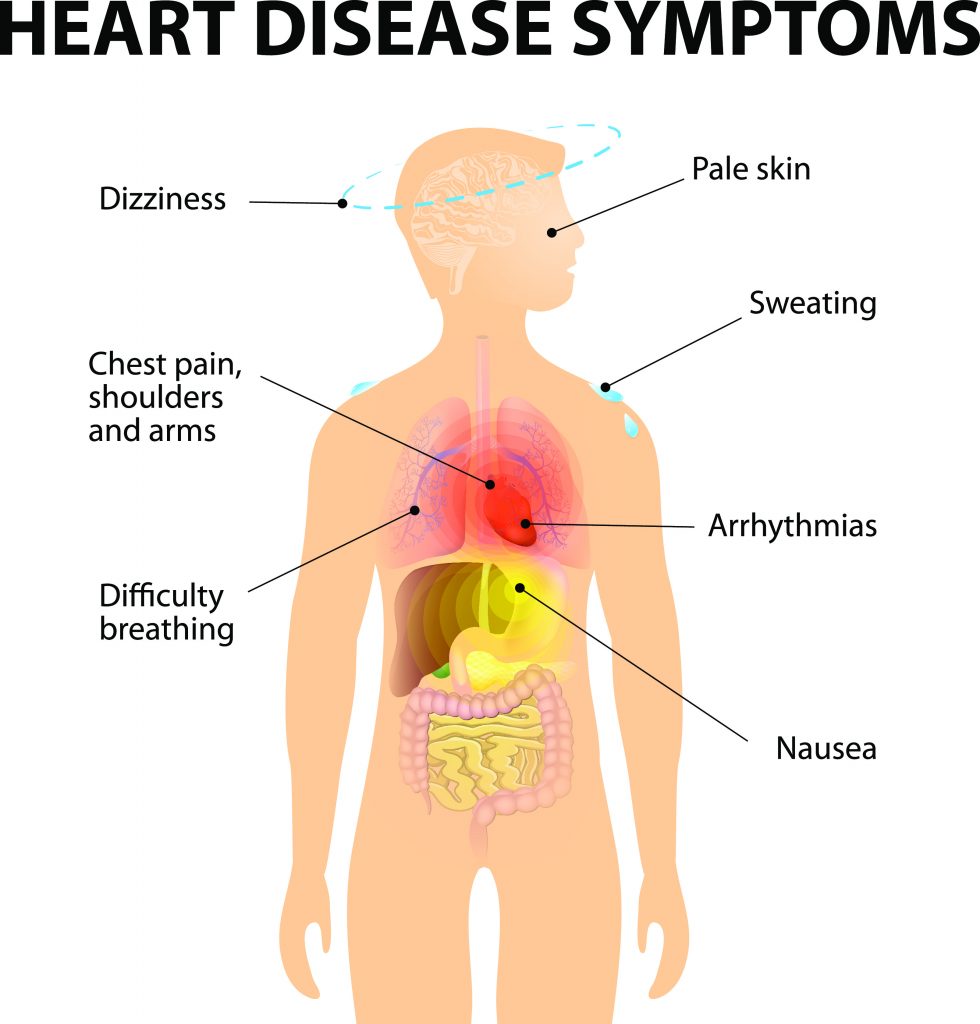
Ageing causes a general failure of energy utilisation in the body and thus in the heart it first causes impaired relaxation of the heart leading to relaxation or diastolic heart failure (HFpEF) – heart failure with preserved ejection fraction.
Symptoms such as breathlessness and swelling of the feet may be seen. A thorough evaluation, including the use of Two Dimensional Echocardiography, will reveal the diagnosis and this can be treated with medication.
A more serious situation arises when the heart muscle is damaged by heart attacks, uncontrolled hypertension, diabetes and other disorders. The underlying cause needs to be identified and appropriate treatment instituted. A Two dimensional Echocardiogram will reveal a low ejection fraction of less than 40 %—( HFrEF; — heart failure with reduced ejection fraction).
To support the heart muscle there are excellent new drugs available (ARNI and SGLT2i) In certain cases one may consider, when appropriate, valve replacement, cardiac re-synchronisation therapy and heart transplant where appropriate.
With periodic evaluation and appropriate life style modification and treatment, a very significant number of heart failure cases can be adequately treated.
Ageing of the Heart Valves:
The normal heart valves are thin and pliable. They allow unidirectional flow of blood. With advancing age they become thick and rigid with restricted mobility. They may also start leaking. The aortic and mitral valves are most commonly affected leading to a strain on the left side of the heart. This manifests as breathlessness, light headedness and sometimes chest pain.
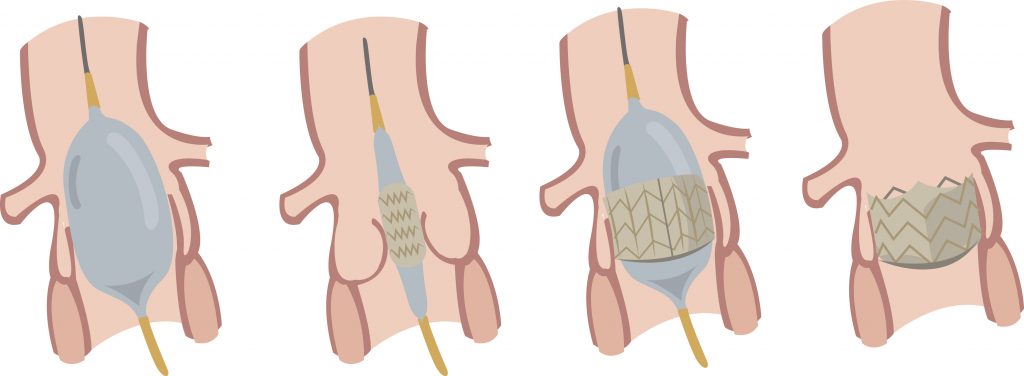
If valve dysfunction is severe then the valve may have to be replaced.
Surgical replacement of the diseased valve and occasionally a valve repair have been the main treatment modality (open heart surgery). Recent advances in technology now permit the aortic valve to be replaced without open heart surgery. The technique is called TAVR — Transcutaneous Aortic Valve Replacement. This technique is now available in Mumbai.
Transcutaneous Mitral Valve Replacement / Repair is in the pipeline and will be available in the not too distant future.
Senescence of the Electrical Generating and Conduction System of the Heart:
The heart generates its own electricity. The powerhouse or pacemaker is situated in the right upper chamber of the heart. From here the electric impulse spreads along specialised “wires” to reach the upper and lower chambers of the heart. There is a special transmission station between the upper and lower chambers called the A-V node. The lower chambers receive electricity via the left and right bundle branches.
Failure of the Power Generator (Sinoatrial Node) is called Sick Sinus Syndrome and can lead to sudden stoppage of the heart for a few seconds causing blackouts and sometimes death.
There can also be various types of fast or slow abnormal heart rhythms. After evaluation many patients may need a Permanent Pacemaker together with medicines to control fast heart rhythms.
A not uncommon abnormality is an abnormal heart rhythm called Atrial Fibrillation (AF) The upper chambers contract at rates above 350 / min and there is no meaningful contraction of the upper chambers. Blood stagnates in these chambers and clots—these clots are then propelled into the circulation where they can cause major strokes and other organ or limb dysfunction. AF needs to be identified by various methods, particularly if it is intermittent, like Ambulatory ECG monitoring. Once identified, the arrhythmia needs to be controlled with medications or other Electrophysiological treatment. The patient will have to take lifelong Anticoagulants —blood thinners—to prevent clots in the event of AF recurring.
The conduction system of the heart can undergo age or disease related dysfunction. This will primarily manifest as blackouts / sudden death. The treatment is to implant a Permanent Pacemaker.
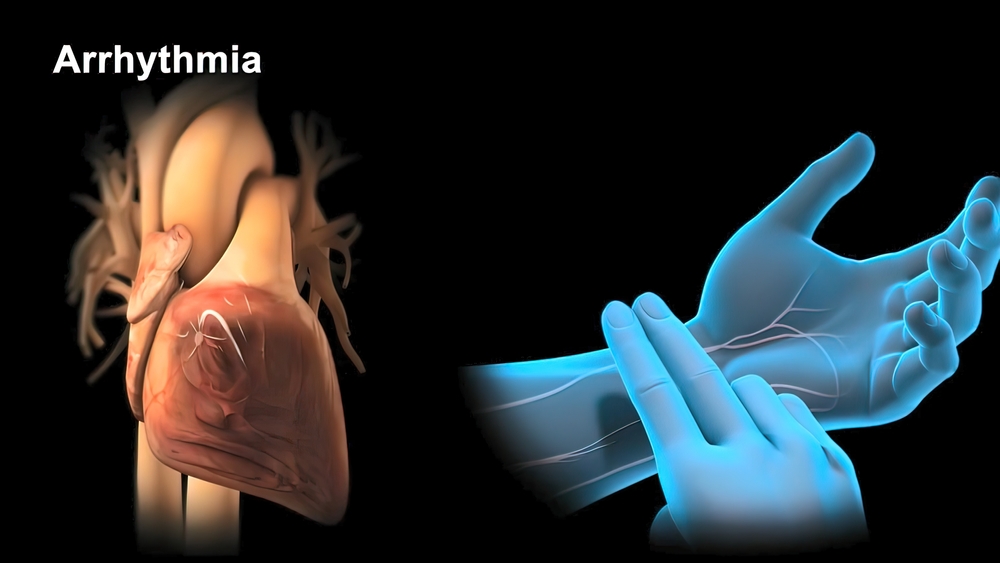
Serious electric disturbances (Ventricular Tachy-Arrhythmia) can occur when the heart muscle is damaged by lack of blood supply, a disease process or there is an unstable electric substrate from birth. These lethal arrhythmias may be treated with powerful drugs or need the support of an Implanted Cardioverter Defibrillator (ICD) which will provide a shock to the patient’s heart if the lethal arrhythmia should occur. This can be lifesaving. These devices are routinely used in India.
Ageing and Atherosclerotic Coronary Vascular Disease (ASCVD):
This is now increasingly manifest in young adults but is often seen in Senior Citizens.
Atherosclerosis or hardening of the arteries occurs when there is damage to the inner lining (endothelium) of the blood vessels that exceeds the capacity of the natural reparative process of the body to effect a perfect repair. This imperfect repair permits cholesterol and other fatty substances to enter the inner lining of the blood vessels and initiate a process of inflammation and further endothelial damage and deposition of fatty substances leading to more luminal compromise, lack of blood supply and ultimately organ damage.
Many patients have a strong genetic history of atherosclerosis but most have risk factors like diabetes, dyslipidemia, hypertension, obesity , tobacco abuse and so on.Every effort is to be made to improve lifestyle, control risk factors as outlined above to prevent and treat atherosclerotic coronary heart disease.Patients with ASCVD may experience chest pain on exertion (angina), breathlessness, fatigue, palpitations or have no symptoms whatever.
Some individuals may end up with an acute heart attack (AMI).In the event of an acute heart attack—— reach a hospital ASAP as it is vital to restore blood supply to the heart ASAP… There is a Golden Hour —a time window within which restoration of blood supply will minimise damage and therefore it is advisable to rush to the ER of a hospital in the event of chest pain, uneasiness and breathlessness. Do not think it is “gas” or indigestion. Let the ER physician make that decision. If a diagnosis of a heart attack is made, the doctors after initial and quick evaluation will suggest a Primary Angioplasty in the Cardiac Catheterisation Laboratory or Thrombolysis (Clot Buster Injection) to restore blood flow. In the worst case scenario a Coronary Bypass Surgery may be advised. These treatments are very effective, the standard of care and much safer than doing nothing. Further treatment will be administered after the blood supply is restored.
For Chronic Lack of Blood Supply to the heart— the doctors may suggest several tests and if required a coronary angiogram to quantify the problem. The quantum and the nature of the blocks will decide the necessity / suitability for Coronary Angioplasty, Coronary Bypass Surgery or Aggressive Medical Treatment. Whichever treatment is suggested, lifestyle modification and control of risk factors is essential.
The subject of ageing and the Cardiovascular System is a vast and complex one. In this article I have distilled its essence in simple terms for the general reader.
Dr Eric Borges
Interventional Cardiologist
Bombay Hospital, Mumbai



