The Big O, osteoporosis, is among the things we dread as we grow older. Dr Darius Soonawalla tells us what is osteoporosis, and how to manage it
Osteoporosis is a condition that results in loss of bone strength, making bones fragile and more prone to fracture.
It occurs when bones lose minerals and proteins, more quickly than the body can replace them. This leads to loss of bone thickness (also called bone mass or density). This is a normal part of ageing for everyone.
About normal bone strength
Normal bone also contains collagen, a protein that forms the physical framework of bone. On this framework is a mixture of minerals like calcium, phosphorus and magnesium, giving the whole frame strength and rigidity.
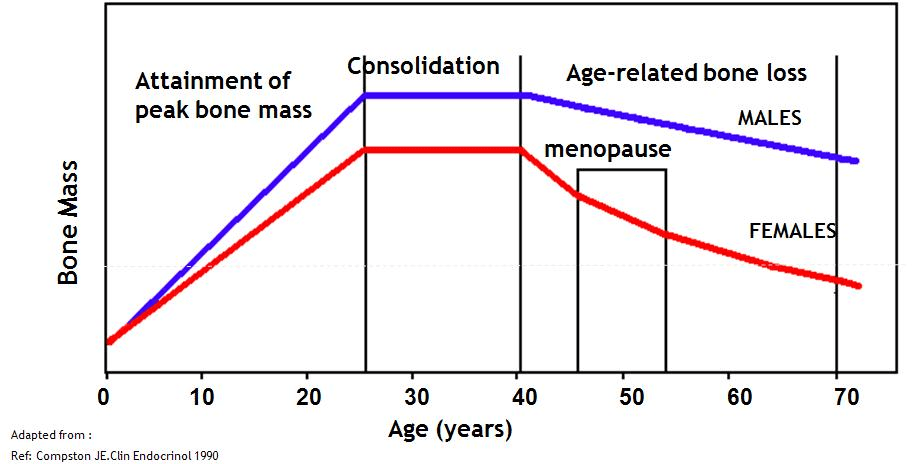
Bone is constantly being broken down and reformed. From birth upto age 25, bone is largely built up and little broken down. From our mid 30s onwards, more bone is broken down than formed. This results in a gradual decrease in bone strength as we age.
Hormones such as oestrogen play a role in maintaining bone strength. When women go through menopause there is a significant fall in oestrogen. This means there is rapid bone loss in the years immediately after menopause. However, the rate of loss slows 4-8 years after menopause. This is why osteoporosis affects women much more.
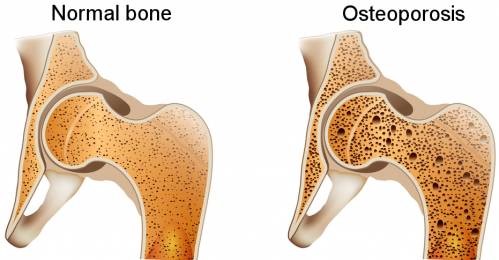
With osteoporosis bones become thinner and brittle, and in severe cases even a minor bump can cause a fracture (break or crack). Any bone can be affected by osteoporosis, but the most common sites are the spine, hip, wrist, ribs, pelvis and upper arm.
Often, there are no signs or symptoms of osteoporosis until a fracture occurs. This is why osteoporosis is called the “silent thief”.
A loss in height or an increasing stoop may be signs of osteoporosis.
What is Osteopenia?
Osteopenia is essentially lower bone density, where bones have lost some mass and strength. In osteopenia the bone density is between normal bone density and osteoporosis. A woman with osteopenia has a risk of broken bones that is higher than normal, but not as high as with the more severe effects of osteoporosis.
Osteoporosis in India
The Osteoporosis society of India estimated the number of osteoporosis patients at approximately 36 million in 2013.
The commonest fracture due to osteoporosis is in the spine, affecting 60% of women above 80 years. The second most common osteoporosis fracture involves the hip, affecting 25% of women above 80 years.
Besides normal ageing, poor lifestyle, certain illnesses or hormonal ad nutritional deficiencies can also cause osteoporosis. These risk factors help in identifying people more likely to develop osteoporosis.
| CAUSE | EFFECT ON BONE HEALTH | |
| Family history | You are at increased risk of osteoporosis if you have a family member with osteoporosis, especially a parent or sibling who has had a hip fracture. | |
| Physical inactivity | Lack of physical activity reduces bone and muscle strength. | |
| Calcium | A lack of calcium in the diet weakens bones. | |
| Vitamin D | Low vitamin D, due to inadequate sunlight, can reduce the body’s ability to absorb the calcium. | |
| Low oestrogen | A drop in oestrogen causes a loss in bone strength
late onset of menstrual periods absent or infrequent menstrual periods early menopause |
|
| Eating disorders | Malnutrition cause a loss of bone strength. It also affects hormone levels which results in bone weakening. | |
| Alcohol | Excessive alcohol intake increases the risk of developing osteoporosis. | |
| Smoking | Excess smoking cause a significant reduction in bone density. | |
| Hypopituitarism- pituitary gland failure |
Hypopituitarism can cause a deficiency in cortisol and the usual treatment is long-term replacement with steroids. This causes Osteoporosis. | |
| Hyperthyroidism- overactive thyroid | High levels of thyroid hormone can lead to more bone breakdown than bone formation and causes osteoporosis | |
| Chronic diseases | Certain diseases, and sometimes their treatments, affects bone strength including chronic liver disease, chronic kidney disease, coeliac disease, diabetes, rheumatoid arthritis and asthma. | |
| Drugs | Certain therapeutic drugs cause bone weakening
steroids chemotherapy drugs used in cancer some drugs used in epilepsy a diuretic Furosemide heparin |
|

Vertebral (spinal) fractures
Spinal fractures are common with osteoporosis and can cause significant pain or lead to distortion, particularly the development of a stooped posture (kyphosis). Some spinal fractures may lead to no symptoms or signs, with women being unaware that they have had a fracture. Changes in posture can also increase the risk of a fall or lead to difficulty with digestion or breathing. In addition, people who have had spinal fractures are more likely to have further fractures in the future.
Hip fractures
Hip fractures are often the result of osteoporosis, particularly if you are over 75 years of age.
Hip fractures require hospitalization and surgery. Recovering from a hip fracture and surgery can be long and painful and may mean there is some permanent loss of mobility. This loss may lead to reduced independence or the need for long term care and you may be more likely to have further fractures in the future.
Complications can arise in the elderly following surgery for hip fracture, and these are associated with an increased risk of death, so follow-up medical care is critical.
Wrist fractures
Wrist fractures can occur with a fall onto an outstretched hand, and can result in immobility, inconvenience and loss of function, especially if the fracture occurs in the dominant hand (ie your right hand if you are right-handed).
Other fractures

If you have severe osteoporosis, minor trauma such as sneezing, coughing, minor knocks to limbs or minor falls can lead to fractures. Therefore, any fractures resulting from minor trauma should be investigated to determine whether there is underlying osteoporosis.
How is osteoporosis diagnosed?
To assess your bone density and risk of developing osteoporosis, your doctor may ask you questions linked to the causes of osteoporosis including:
| LINKS TO OSTEOPOROSIS | QUESTIONS YOUR DOCTOR MAY ASK |
| Alcohol | How many alcoholic drinks do you have per day?
Do you have alcohol-free days each week? |
| Calcium | What was the level of calcium-rich foods (such as milk, yogurt, broccoli, beans, almonds or salmon) you had as child and teenager?
What is the current level of calcium-rich foods in your diet? How many caffeinated drinks do you have each day? How much salt do you have each day? |
| Corticosteroid therapy |
Are you taking, or have you ever had to take, a course of:
prednisolone cortisone hydrocortisone dexamethasone? |
| Exercise | How much exercise do you do in an average week? |
| Family history | Is there anyone in your immediate family (mother, father, sibling) who has had osteoporosis or fractures, and at what age were they diagnosed? |
| Fracture | Have you suffered any fractures? |
| Hyperthyroidism (overactive thyroid) | Have you ever had any thyroid problems? |
| Medication | What medications do you take? |
| Menopause | Are you experiencing any of the symptoms of menopause?
Have your periods stopped and when did you last have a period? |
| Menstruation | At what age did your periods start?
Are your periods regular? |
| Posture | Have you noticed a change in your posture or loss of height? |
| Smoking | Do you smoke and if so, how many cigarettes do you smoke per day?
If you smoked in the past, when did you stop smoking? |
If your doctor finds you have significant risk factors for osteoporosis, then your doctor may arrange tests as outlined below.
DXA scan
A dual energy X-ray absorptiometry scan (DXA, previously DEXA) is a specialised X-ray used to measure bone mineral density.
A DXA scan may be used to:
confirm a diagnosis of osteoporosis
identify the extent of any bone loss
determine whether any treatment for osteoporosis is working
What to expect when you have DXA scan
Having a DXA scan is a similar process to having a normal ‘X-ray’. It does not hurt, is fast and has a lower radiation dose compared to other X-ray methods.
Usually only the bones in the lower back (lumbar spine) and hip region (proximal femur) are measured. In special cases the bones in your forearm (radius) may be measured.
Understanding your results
The result of a DXA scan is presented as a T-score and Z score
Your T-score reflects how much your bone density differs from that of a healthy young person (when peak bone mass is at its best), measured in ‘standard deviations’ (the average distance from the average). A negative T-score means you have reduced bone density which will happen as you age. It is the extent of the negative score that is important to consider.
The stages and progression of bone mineral density loss from normal to osteopenia to osteoporosis are:
| T-SCORE RANGES | |
| Normal bone density | -1.0 to 0 |
| Bone density for osteopenia (thinning of the bones is present but there is no increased risk of fracture) | -1.0 to -2.5 |
| Bone density for osteoporosis (thinning of the bones is present and there is an increased risk of fracture) | -2.5 or less |
Assessing the risk of fracture
A low bone mineral density measure is associated with an increased risk of fractures. For every reduction in T-score, the risk of fracture doubles so someone with a T-score of -2 faces twice the risk of fracture compared with someone whose T-score is -1.
Other risk factors mentioned earlier also influence the likelihood of fracture, not just the bone mineral density reading on a DXA scan.
Frequency of DXA scans
Generally your doctor will arrange for you to have a repeat DXA scan every two or three years to monitor the status of your bones and/or assess the effects of therapy.
X-ray
A plain X-ray of your upper and lower spinal column (thoraco-lumbar spine) may be ordered to determine whether there are already features of osteoporosis affecting the spinal column. Up to one third of women with osteoporosis may have had a fracture of the spine without knowing it.
Blood tests
It may also be necessary to have blood and urine tests to look for any contributing causes for osteoporosis. This may include assessment of vitamin D levels, calcium levels and thyroid function.
Ultrasound
Currently ultrasound measurement of the heel is available to diagnose osteoporosis. Ultrasound tests are not as accurate in assessing for osteoporosis as a DXA scan.

Management & treatment
In youngsters it is important to achieve a high peak bone mass with exercise and a healthy diet. After that bones usually weaken with age, so the focus from early on is to prevent bone loss, maintain existing bone strength, and treat existing osteopenia (before the bones develop osteoporosis) and osteoporosis.
Lifestyle management
A diet that includes: Calcium, limited caffeine, limited alcohol, adequate vitamin D and 45 min of sunlight exposure per day, calcium and vitamin D supplements if you have a deficiency, physical activity – especially weight-bearing exercise, not smoking, and fall prevention strategies in the elderly.
Illnesses & medications
If you have an illness or take medication, which increases your risk of osteoporosis, it is important to be aware of this impact, discuss the effects with your doctor, and have regular testing of your bone density.
Medical management of bone health
Oral contraceptive pill (OCP)
| Who might be helped by taking the OCP | The OCP may help extreme athletes, women with current eating disorders, or those with low oestrogen levels for other reasons who have either stopped having their periods, or have periods very infrequently. A lack of periods is associated with low oestrogen levels, which reduces bone density. |
| How it works | Using the OCP can restore oestrogen levels to normal, and research has shown that this may allow bone density to be better preserved. |
| Possible side effects/risks | There is a small increased risk of deep vein thrombosis (DVT) (blood clots in the veins) with the OCP
Women who smoke should not take the OCP as the risk of DVT is increased It is not clear whether the OCP improves bone mass in those with already lowered bone density |
Hormone replacement therapy (HRT)
| Who might be helped by taking HRT | HRT can help women at the time of menopause because with menopause there is a dramatic fall in oestrogen levels and the loss of bone is accelerated. |
| How it works | HRT can lead to higher levels of oestrogen which can increase bone density. |
| Possible side effects/risks | The use of HRT is for menopause symptoms and is not currently recommended as a first line therapy for osteoporosis in postmenopausal women
HRT has been linked to a slight increase in risk of breast cancer after 4-5 years of use in those who take combined oestrogen and progesterone The effects of HRT last only whilst you are taking it and as soon as you stop, the rate of bone loss returns to the rate it was progressing before you started HRT |
Bisphosphonates
Taking bisphosphonates can assist men and women at high risk of fracture, with a history of low trauma fracture and who have other risk factors for osteoporosis.
There are several kinds of bisphosphonates:
Tablets (weekly or monthly)
Alendronate
Risedronate
Intravenous infusion (once yearly)
Zoledronic acid
| How they work | These medications are taken up by the skeleton and reduce the rate of bone loss
Bisphosphonates reduce the risk of spinal and hip or other fractures These drugs usually become effective within 6-12 months |
| Possible side effects/risks | They are generally well tolerated
Acidity Heartburn abdominal discomfort ulceration of the oesophagus – but when taken correctly the chance of oesophageal ulceration is low |
For bisphosphonates to be effective in increasing bone mineral density, it is important to have an adequate intake of calcium and vitamin D. It is also important to have a dental check-up and tell your dentist you are taking bisphosphonates as they can affect the bone in your jaw if you need to have a tooth removed.
Raloxifene (brand name Evista)
Taken as a daily tablet
| How it works | This is a selective oestrogen-receptor modulator drug or SERM that improves bone density and reduces the risk of spinal fractures
It acts like oestrogen at some sites in the body and as an anti-oestrogen in other sites (such as the breast and uterus and so reduces the risk of breast cancer) |
| Possible side effects/risks | Hot flushes, which can make it difficult for women who are going through menopause
There is a slightly increased risk of deep vein thrombosis (DVT or blood clot in a vein deep in the body), so if you are going to be immobile for some time such as a long air trip you should get your doctor’s advice about whether to stop this treatment |
Other medications
Other medications used to treat osteoporosis include:
| MEDICATION | WHO THEY WORK FOR | HOW TO TAKE | POSSIBLE SIDE EFFECTS/RISKS |
| Strontium Ranelate | Moderate & severe osteoporosis. | Taken daily as granules mixed with water. | Should not be used in those at significant risk of cardiovascular events, unless otherwise advised by their doctor. |
| Parathyroid hormone (PTH) – Teriparatide ( | Patients with severe osteoporosis who have already been on other osteoporosis medications | A daily injection for 18 to 24 months. | There may be an increased risk of bone cancer with long-term use. |
| Denosumab ( | Severe osteoporosis. | An injection given twice a year. | There may be a slightly increased risk of skin infections. |
For information on any medications to treat osteoporosis you should see your doctor.
Calcium
The importance of calcium
Calcium is one of the essential nutrients necessary for healthy bone development. Bones contain most of our body’s calcium, so they act as the body’s ‘reservoir’ of calcium. Calcium is critical for the function of cells in the body and a certain amount of calcium circulates within the blood, with the body maintaining the levels of calcium within a very tight range. Our bodies cannot make calcium, and if blood calcium levels fall, the body will compensate for this by drawing calcium out of bones and putting it into the blood. Calcium is also excreted by the body daily.
This means it is important to have an adequate daily intake of calcium through your diet, so your bone mineral strength is not compromised.

Recommended daily calcium intake
There are critical times in life when it is vital to ensure that calcium intake through food and/or supplements is adequate and meets the recommended requirements. The following table lists these requirements:
| WHO | AGE | RECOMMENDED DAILY CALCIUM | BONE HEALTH ISSUES |
| Children | 1-3 | 500mg | During this growth phase the foundations for peak bone mass are laid, so it is essential calcium intake matches the needs of growing bones. |
| 4-8 | 700mg | ||
| 9-11 | 1,000mg | ||
| 12-18 | 1,300mg | ||
| Adults | 19-50 | 1,000mg | Between 20-30 years bone gain and loss is quite stable – a healthy lifestyle during these years supports good bone health
From the mid-30s onwards, bone loss starts to increase more than bone gain |
| 50+ | 1,300mg | When women go through menopause, there is a rapid loss of bone because of decreased oestrogen and this process may last from 4-8 years after menopause
After this period of time the rate of bone loss is reduced and stabilises The gastrointestinal system and kidney become less efficient at absorbing and conserving calcium in the body and this creates a state of potential calcium loss in the blood so the body compensates for this by drawing calcium out of the bones The reduced exposure to sunlight and lower vitamin D levels of many women over 50 can reduce the absorption of calcium for bone strength |
|
| Pregnant and lactating women | 14-18 | 1,300mg | Pregnant women and breastfeeding women have higher requirements for calcium to be absorbed through the mother’s gastrointestinal system. The calcium is needed to support:
skeletal growth of the foetus milk production Normal pregnancy and breastfeeding is associated with a certain amount of bone mineral loss, which generally recovers 6-12 months after birth and/or stopping breast feeding[1] |
| 19-30 | 1,000mg | ||
| 31-50 | 1,000mg |
Source: National Health and Medical Research Council. (2006) NZ
Calcium content of various foods
While dairy products can provide a good source of calcium, daily calcium requirements need not necessarily come only from these. Two serves of dairy products and another serve of calcium-rich foods like broccoli, beans, almonds, tinned salmon and sardines equate to about 1,000mg of calcium.
If you choose alternative calcium sources, note the quantity of calcium found within the particular food source. The following table lists the average calcium content of a variety of foods:
| FOOD | SERVING | CALCIUM PER SERVE |
| Regular milk | 1 cup (250ml) | 285mg |
| Skim milk | 1 cup (250ml) | 310mg |
| Natural yogurt | 1 tub (200g) | 340mg |
| Low fat yogurt | 1 tub (200g) | 420mg |
| Cheddar cheese | 40g cube | 310mg |
| Low fat cottage cheese | 100g | 80mg |
| White bread | 1 slice | 15mg |
| Cooked spinach | 1 cup (340g) | 170mg |
| Cooked broccoli | 1 cup (100g) | 30mg |
| Canned salmon (+ bones) | ½ cup | 230mg |
| Canned sardines (+ bones) | 50g | 190mg |
| Almonds | 15 almonds | 50mg |
| Tofu | 100g block | 0-100mg* |
* The calcium content of tofu depends on how the tofu has been processed. If it is processed using calcium chloride or calcium sulphate, tofu may have up to 100mg calcium per 100g block. Otherwise the calcium content of tofu is very low.
Calcium supplements
Calcium needs are generally best met through diet. However, calcium supplements may be required by those who do not obtain adequate calcium from food products to meet the 1,000-1,300mg per day required for girls and women.
Most calcium supplements in Australia contain:
calcium carbonate (sold as caltrate) or
calcium citrate (sold as citracal)
Calcium carbonate
Caltrate requires an acidic environment for maximum absorption and should be taken with meals.
Calcium citrate
Calcium citrate does not require an acidic environment and therefore can be taken on an empty stomach (but is better taken with food). It is the preferred calcium product for people who need to take anti-reflux medications.
When to take calcium supplements
It is best to take calcium supplements at night, as this is when bone ‘turnover’ increases.
High dose calcium supplements may be linked with heart disease. Beneficial effects of calcium are found with relatively low doses (500-600mg). Elderly individuals and others with impaired kidney function may be at higher risk of cardiovascular disease.

Vitamin D
Vitamin D has many important roles in the body including helping with calcium absorption, cell growth and maintaining a healthy immune system to fight disease and illness. Find out about these important roles as well as vitamin D deficiency, how to test for vitamin D deficiency and where to get vitamin D.
The importance of vitamin D
Vitamin D is essential for bone health. It helps increase the absorption of calcium from the stomach, regulates the amount of calcium in the blood and strengthens the skeleton.
The main source of vitamin D is production in the skin after exposure to sunlight. Small amounts of vitamin D are available in some foods. For vitamin D to work effectively it needs to be activated by the liver and kidney, which then turns it into a hormone.
Vitamin D has many roles within the body. The most understood role is its ability to help the body absorb calcium and phosphorus and vitamin D also assists with bone development and strength, cell growth, maintaining a healthy immune system, hormone function, and nervous system regulation.
Apart from its important role in maintaining bone health, vitamin D may also have an important role in other diseases such as diabetes, cancer and infection. These are currently areas of intense research.
Vitamin D deficiency
Vitamin D deficiency is a common condition in Australia, affecting a large number of women.
The body’s main source of vitamin D comes from the skin being exposed to UV radiation in sunlight. When sunlight hits the skin, it reacts with a cholesterol-like substance and produces vitamin D. The amount of sun exposure needed depends on your skin colour, where you live and the time of year.
Even though Australia has one of the highest UV radiation levels in the world and is well known for its abundance of sunshine, research has found many people are deficient in vitamin D because of the amount of time they spend indoors.
Those at most risk of having a vitamin D deficiency include:
- older people and people living in care (such as hospitals or rehabilitation) – particularly those who stay indoors or cannot walk and have limited exposure to the sunlight
- people with gastrointestinal disease
- people taking certain medications (e.g. anti-epileptics)
- people who cover or veil their skin for religious or cultural reasons
- dark-skinned people
- pregnant women
- postmenopausal women
Vitamin D levels are seasonal and fall in the winter and early spring when people are less likely to be outdoors.
How do you know what your vitamin D level is?
Vitamin D levels can be measured through a simple blood test.
Vitamin D levels are classified into ranges. The Australian and New Zealand Bone and Mineral Society, the Endocrine Society of Australia and Osteoporosis Australia (2005) state that adult serum 25-OHD levels show:
| LEVEL OF VITAMIN D DEFICIENCY | RANGE (IN NMOL/L – A MEASURE OF THE MOLECULAR CHEMISTRY) |
| Mild | 25-50 |
| Moderate | 12.5-25 |
| Severe | Less than 12.5 |
Where to get vitamin D
| WHAT YOU NEED | WHAT TO BE CAREFUL OF |
| Sunlight | |
| Usually 10-15 min exposure to outdoor sun per day is necessary for the production of adequate vitamin D. As a general guide expose face, arms, hands or legs for:10 minutes in summer5-20 minutes in spring and autumn30 minutes in winterCheck the map of Australia for guidelines on the recommended amount of sun exposure based on your location, the season and your skin pigmentation. You can get daily updates on the UV index at: sunsmart.com.au |
Avoid excessive exposure to sunlight, particularly in summer because of the risk of skin damage and skin cancers
Don’t use solariums as a substitute for sunlight because the UV radiation in solariums: doesn’t help to produce vitamin D will not help with vitamin D deficiency increases your risk of skin cancer |
| Diet | |
| Dietary sources of vitamin D are limited and can come from:
plants (vitamin D2) such as mushrooms – shitake and button mushrooms are good options animal sources (vitamin D3) such as liver, fish (tuna, salmon, sardines, herring and mackerel) and egg yolk – one egg can supply 10% of your daily intake fortified foods (boosted) with vitamin D such as milk, soy drinks, margarine, breads and cereals |
It is very hard to get adequate amounts of vitamin D from these sources alone. |
| Supplements | |
| For the elderly who are in care, taking additional vitamin D supplements and calcium supplements may reduce the incidence of fracture[1]. | Get your doctor’s advice about whether to take a vitamin D supplement after you have been tested. |
What you need to know
Vitamin D helps with bone health
Exposure to sunlight each day is important to maintain vitamin D levels
See your doctor to have a blood test to determine your level of vitamin D
If you are vitamin D deficient, it may be necessary to take a vitamin D supplement
Your treating doctor can recommend whether you need to take a vitamin D supplement
Healthy living & bone health
One way to increase your chances of having healthy bones is to have a healthy lifestyle. Below you will find information on the management of bone health through a healthy diet such as the foods to include with calcium, vitamin D, phosphorous and protein. There are also tips on the best exercises for bone health and what to do before you start an exercise program.
The following general information provides a summary for management of bone health through having a healthy lifestyle.
Diet
| INFLUENCES | WHAT TO DO |
| Healthy eating | Include in your daily diet:
cereals vegetables legumes (lentils, beans) fruit milk, yoghurt, cheese lean meat fish poultry nuts |
| Calcium | To meet your calcium needs, include in your daily diet:
2 serves of dairy foods a serve of calcium-rich foods – e.g. broccoli, beans, almonds, tinned salmon or sardines |
| Vitamin D | To meet your vitamin D needs in order to have normal absorption of calcium, choose foods that are known to have higher levels of vitamin D such as mushrooms, fish, liver and egg yolks. |
| Protein and phosphorus | Protein intake is important for bone development as it provides the necessary building blocks in bones. High-protein foods include beef, veal, lamb and pork, chicken and turkey breast, tuna and soy beans.
Phosphorus is a mineral and nutrient we all need for strong bones and proper cell functioning. Phosphorus is found in milk, grains like rice and oat bran, seeds, bacon and protein rich foods. Diets that are very high in protein and phosphorus can disrupt the calcium balance causing the body to take calcium from the bones. If you have an adequate calcium intake, then the effect of high protein and phosphorous is not as significant, which means adequate calcium intake is a priority. |
| Caffeine and salt | High intake of salt and drinking more than three caffeinated drinks per day can reduce calcium absorption. In addition, people who drink very high quantities of caffeine also tend to eat/drink less calcium rich foods and drinks.
If you suspect your salt or caffeine levels may be too high, it can be helpful to see a dietitian even for one visit to work out some alternatives |

Physical activity & exercise
Weight bearing & high impact activities
Weight bearing exercise, which is exercise done while on your feet so you bear your own weight and support your skeleton, is the key to good bone health. This includes fast paced walking (to have an effect on your bones), running, tennis or dancing. Walking at a fast pace and jogging have been found to help strengthen bone mass – sedate and slow walking may not be as protective of bone.
High intensity, rapid impact exercise stimulates bone cell formation. This form of exercise generally refers to weight bearing exercise that involves more load placed through the leg bones and spine, during landing after lifting one’s own body weight off the ground. Examples of this include running, skipping, jumping, high impact aerobics and team sports such as netball.
Fifteen minutes of weight bearing exercise, four times per week is helpful for bones. This might include gym resistance training (set by a trained instructor), medium impact aerobics, skipping, dancing, and jumping exercises.
Certain physical activities can increase your risk of fracture, so any exercise activity should first be discussed with your doctor.
Strength training
These activities are also known as resistance exercises. Strength training uses weights of some kind (e.g. machines, dumbbells, ankle or wrist weights) to create resistance, which helps to build muscle mass. It includes activities that use one’s own body weight as the load (e.g. push-ups, where load is placed through the arms and shoulders).
Load placed on bone leads to increased bone formation at the site where the load is greatest. The benefit is site specific, so if you are using weights on your legs, it only benefits your leg bones.
Ideally strength training programs should be performed regularly, 2-3 times per week. Strength training is most beneficial when a small number of repetitions (e.g. 8-12) are used, and the weight is progressively increased. As your strength improves, it is best to increase the weight used in the exercise rather than increasing the number of repetitions.
There is evidence to suggest high impact loading and resistance type/strength training activities probably provide the most benefit for improving bone mineral density.
Physiotherapy
A physiotherapist can provide assistance with bone strengthening exercises and fall prevention by addressing posture, balance, coordination and muscle strength.
If you have had a fracture, a physiotherapist or exercise physiologist can tailor an exercise program to suit your needs as part of your rehabilitation.
Hydrotherapy
Using warm water activities is particularly beneficial if you need to be careful with exercise. The buoyancy of the water allows for easier movement and less chance of pain. Supervised muscle strengthening exercises can help both rebuild bone and improve balance and posture, thereby assisting in the prevention of falls.
Risky exercises if you might suffer a fracture
If you have osteoporosis it may be best to avoid some of the following exercises:
| TYPE OF EXERCISE | EXAMPLE |
| Dynamic abdominal exercises | Sit ups |
| Twisting movements | Golf swings |
| Trunk flexion | Bending forward |
| Sudden jerking movements | Tennis |
| High impact exercise | Jumping |
Source: Everybody’s bones: a handbook for the prevention and management of osteoporosis (3rd edition), Osteoporosis Australia, 2001
Activity programs
| Before you start | If you have not been active regularly, see your doctor before you start any exercise or physical activity program
If you have osteoporosis, see your doctor and seek advice from a physiotherapist or exercise physiologist |
| Starting your program | Start slowly and progress gradually
Choose something you enjoy Join a group or a gym Wear appropriate footwear such as supportive runners |
| Keeping your program on track | Vary your activity
Get active with a friend – start a walking group, join a line dancing group or take up yoga or Tai Chi Pay up front for activities that incur a cost to motivate you to keep going Keep an activity diary and schedule your activity at the start of each week Match your activity to the weather and seasons – outdoor walking, gardening, Tai Chi for warmer weather and indoor line dancing, gym and yoga for cooler weather Listen to your body – if there is any pain, seek professional advice |
If any pain is experienced during exercises, the exercises should be stopped and if the pain persists you should consult your doctor.
A word on excessive exercise
If you do not have periods, the emphasis of treatment is to restore normal period patterns and this may mean:
changing training routines
if you are underweight, making sure you have an adequate intake of calories from a wide variety of foods
using the oral contraceptive pill to restore oestrogen levels
Smoking & alcohol
Smoking and excessive alcohol are known to have a negative effect on bone health and lead to a significant reduction in bone density. For more information go to smoking or alcohol.

Managing the risk of falls
Falls are a particular problem as you age as they can lead to fractures especially of the hip. Find information on what increases the risk of falls, things you can do for yourself to lower the risk of falls and who to see if you need expert advice on how to lower your risk of falls.
What increases the risk of a fall?
Factors that may lead to an increased risk of a fall, especially for older women, include poor vision, a decreased sense of joint position, poor balance, poor physical strength, and increased frailty.
Actions to minimise the risk of a fall
Frequent falls may lead you to lose confidence in your ability to move and this can affect your sense of independence. It is worth taking action to minimise the risk of a fall. These actions include:
| Lighting | Ensure you have enough lights in and around your home to make navigation in darker areas and at night easier. |
| Furniture | Move small items of furniture to keep the number of things you might fall over to a minimum. |
| Rugs | Limit the number of rugs in your home if they create an uneven floor surface. |
| Stairs | Choose accommodation with a minimum of stairs. |
| Rails and/or mats | Install rails and/or non-slip mats near stairs and slippery surfaces such as the bathroom floor. |
| Shoes | Choose shoes that give you enough support and traction. |
| Medication | Check whether your medications can affect balance because your doctor may be able to find an alternative. |
| Vision | Check your vision regularly to ensure your vision is correct or corrected. |
| Medical check-up | Have a regular check-up so your doctor can assess your bone strength and how you are walking. |
| Balance and muscle strengthening exercises | Get advice from a physiotherapist or join a class at a local community health centre because:
muscle strengthening balance training and Tai Chi exercise have been shown to reduce the incidence of falls |
| Walking aide | If your doctor recommends a walking aide, use it as a preventative measure so you avoid falls. |

If you are falling because you are fainting as a result of a disorder of your heart rhythm you may need to be assessed and treated by a heart specialist (cardiologist).
The use of hip protectors for the very frail elderly may also reduce the incidence of hip fracture although further research on their use is needed.
If you need expert advice:
Physiotherapists can provide assistance with aides for walking.
Occupational therapists or your community health centre can advise you about making your home environment safer.




It is not clear what is recommended daily calcium intake for senior citizens aged 60-80 yrs. Is it 1000 mg or just 400-500 mg as has been mentioned elsewhere (on the net). Please clarify. Thanks.
Comments are closed.