Diverticulitis is a medical condition that affects the digestive system, causing inflammation and infection in the small, bulging pouches called diverticula that form in the lining of the intestine. This condition can be painful and debilitating, impacting a person’s quality of life. Understanding the causes, symptoms, and treatments of diverticulitis is essential for managing and preventing flare-ups.
What is diverticulitis?
Diverticulitis is a condition characterised by the inflammation and infection of diverticula, which are small pouches that develop in the lining of the intestine. These diverticula usually form in the lower part of the large intestine, known as the colon. When these pouches become infected or inflamed, it can lead to various symptoms and complications.
Diverticulitis occurs when the diverticula becomes blocked with stool, causing bacteria to accumulate and leading to infection. The exact cause of diverticula formation is not fully understood, but it is believed to be primarily due to a low-fiber diet. When the diet lacks fiber, the stool becomes harder, requiring increased pressure to pass through the colon. This increased pressure can cause the lining of the colon to bulge out and form diverticula over time.

Causes of diverticulitis
One of the main causes of diverticulitis is a low-fibre diet. When the diet lacks fiber, the stool becomes bulky and difficult to pass, leading to increased pressure in the colon. This increased pressure can cause the formation of diverticula. Other factors that may contribute to the development of diverticulitis include aging, genetic predisposition, and certain lifestyle habits.
As mentioned earlier, a low-fibre diet is a significant contributing factor to the development of diverticulitis. Fiber is essential for maintaining regular bowel movements and preventing constipation. When the diet lacks fiber, the stool becomes hard and difficult to pass, increasing the risk of diverticula formation. In addition to a low-fibre diet, other lifestyle habits such as smoking and lack of exercise can also increase the risk of developing diverticulitis.

Risk factors for diverticulitis
Several risk factors can increase an individual’s likelihood of developing diverticulitis. The primary risk factor is age, as diverticulitis tends to be more common in older adults. The risk increases significantly after the age of 40, and by the age of 60, the majority of individuals will have diverticula in their colon.
Genetics also play a role in the development of diverticulitis. If you have a family history of the condition, you may be more likely to develop it yourself. Additionally, certain lifestyle factors, such as a sedentary lifestyle, obesity, and smoking, can increase the risk of diverticulitis.
Signs and symptoms of diverticulitis
The symptoms of diverticulitis can vary in severity and may include abdominal pain, bloating, fever, and changes in bowel habits. The most common symptom is abdominal pain, which is usually localised in the lower left side of the abdomen. The pain can range from mild to severe and may worsen with movement or pressure. Bloating and a feeling of fullness in the abdomen are also common symptoms.
Other symptoms of diverticulitis may include fever, chills, nausea, and vomiting. Changes in bowel habits, such as diarrhea or constipation, may also occur. In severe cases, complications such as abscesses, bowel obstructions, or even perforations may occur. These complications can lead to more severe symptoms, including severe abdominal pain, rectal bleeding, and signs of infection.

Diagnosing diverticulitis
Diagnosing diverticulitis typically involves a combination of medical history, physical examination, and diagnostic tests. The medical history will include questions about symptoms, duration, and any previous episodes of diverticulitis. A physical examination may include palpation of the abdomen to check for tenderness or swelling.
Diagnostic tests such as blood tests, stool tests, and imaging studies may also be used to confirm the diagnosis. Blood tests can help identify signs of infection, while stool tests can rule out other possible causes of symptoms. Imaging studies, such as a CT scan or ultrasound, can provide a detailed view of the colon and help identify any diverticula or signs of inflammation.
Treatment options for diverticulitis
The treatment for diverticulitis depends on the severity of the condition. Mild cases of diverticulitis can often be managed at home with conservative measures, while more severe cases may require hospitalisation and medical intervention.
For mild cases, treatment may involve rest, pain management, and a clear liquid diet to give the colon time to heal. Antibiotics may also be prescribed to clear the infection. As symptoms improve, a gradual transition to a low-fibre diet is typically recommended to prevent future flare-ups.
In more severe cases, hospitalisation may be required for intravenous antibiotics and close monitoring. In some cases, a procedure called a colon resection may be necessary to remove the affected portion of the colon. This procedure is typically reserved for individuals who have recurrent episodes of diverticulitis or complications such as abscesses or perforations.
Lifestyle changes to manage diverticulitis
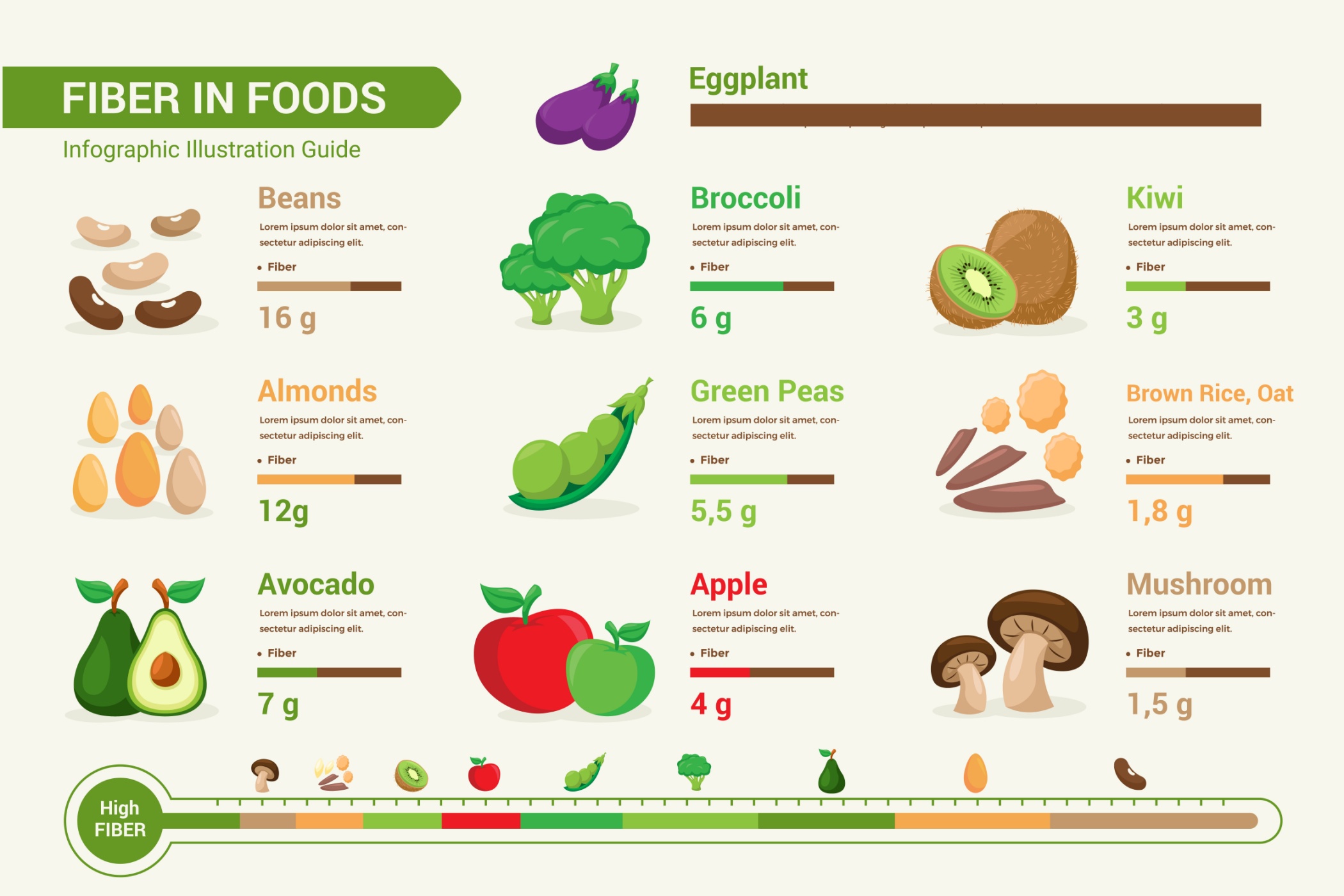
Making certain lifestyle changes can help manage diverticulitis and prevent future flare-ups. One of the most important changes is adopting a high-fibre diet. Fibre helps add bulk to the stool and promote regular bowel movements, reducing the risk of diverticula formation and constipation. Foods rich in fiber include fruits, vegetables, whole grains, and legumes.
In addition to a high-fibre diet, regular exercise can also help maintain a healthy digestive system. Exercise helps stimulate bowel movements and promote overall digestive health. Quitting smoking and limiting alcohol consumption are also recommended, as they can contribute to digestive issues and increase the risk of diverticulitis.

Prevention of diverticulitis
While it may not be possible to prevent diverticulitis entirely, there are steps that can be taken to reduce the risk of developing the condition. One of the most effective measures is adopting a high-fiber diet. By including plenty of fruits, vegetables, whole grains, and legumes in your diet, you can promote regular bowel movements and prevent constipation.
Staying hydrated is also important for maintaining healthy digestion. Drinking plenty of water throughout the day helps soften the stool and prevent dehydration, which can contribute to constipation. Regular exercise, maintaining a healthy weight, and avoiding smoking and excessive alcohol consumption are also recommended to reduce the risk of diverticulitis.
Complications of diverticulitis
While most cases of diverticulitis can be managed with appropriate treatment and lifestyle changes, complications can occur in some individuals. These complications can range from mild to severe and may require medical intervention. Some possible complications of diverticulitis include abscesses, which are pockets of pus that develop in the affected area, bowel obstructions, which can occur when the inflamed diverticula narrow the passage of the stool, and perforations, which are tears or holes in the diverticula or colon.
If any of these complications occur, immediate medical attention is necessary. Treatment may involve antibiotics, drainage of abscesses, or surgery to repair or remove the affected portion of the colon. Early detection and prompt treatment can help prevent further complications and improve outcomes.
Prevent and treat this condition proactively
Diverticulitis is a medical condition that can cause significant discomfort and impact an individual’s quality of life. By understanding the causes, recognising the symptoms, and seeking appropriate treatment, individuals can take control of their health and minimise the impact of this condition. By adopting a high-fiber diet, maintaining a healthy lifestyle, and seeking regular medical care, individuals with diverticulitis can find relief and prevent future flare-ups. With proper care and management, the impact of diverticulitis can be minimised, allowing individuals to lead a healthier and more comfortable life.








