Reading Time: 3 minutes
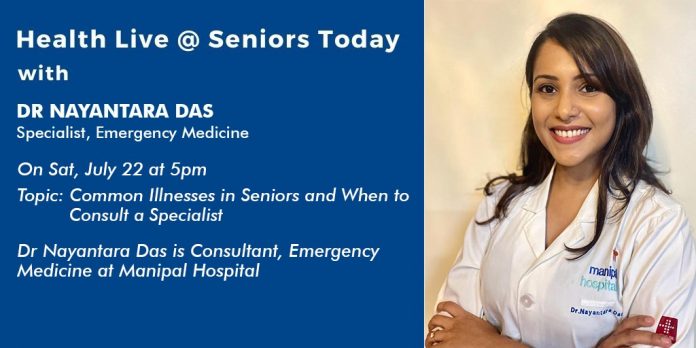
On 22 Jul, 2023, Seniors Today hosted their weekly Health Live Webinar with Dr Nayantara Das, a Consultant in Emergency Medicine at Manipal Hospital who spoke on and answered questions about Common Illnesses in Seniors and When to Consult a Specialist.
Dr Nayantara Das is an ER Physician currently practising at Manipal Hospital, Baner, Pune. Having completed her postgraduate training in the field of Emergency Medicine, she has managed the ER of several multispeciality hospitals in Bengaluru and Pune over the past few years. She specialises in all medical and surgical related emergencies with a special interest in the management of trauma and paediatric emergencies.
Myth: ageing is a disease.
Truth: ageing affects the manifestation of certain diseases and in the process of recovery.
Ageing has/ shows certain subtle changes in every system of the body- nervous system, cardiovascular system, Gi system, and so on and so forth. This is not an indicator of deterioration of health but rather a marker to make changes- in our lifestyle and way of treatment as well.
Special considerations in the senior age group:
- Late presentation/ delayed presentation to the hospital due to increased tolerance to pain and discomfort.
- Atypical/ subtle presentation
- Multiple pathologies and added comorbidities
- Difficulty in extracting an accurate history- due to lacunae at the end of communication, need for a comprehensive and detailed evaluation is necessary.
Common complaints that taken us to the doctor are:
- Fall
- Pain in abdomen, acidity, heartburn
- Constipation
- Dizziness
- Joint pain
- Reduced appetite
- Diminished vision
- Generalised weakness
Some diseases, medical concerns and issues which are seen in the emergency often have a simple solution and require minimum intervention. These are:
- Falls: a fall is never treated as a single entity in an elderly patient. It is treated as a symptom.
30% of falls in the elderly are environmental/ accident related
70% of the falls have an organic cause
Cause and effect of fall are both important. These can be multifactorial, depending on your pre-existing health status, and previously known comorbidities.
Falls need to be paid attention to- if there is a history of recurrent falls, in a short period of time. If the patient does not recall falling/ gives a history of loss of consciousness.
You can perform the “Get up and Go” test on someone who has endured a fall, to evaluate the gravity of the situation and whether the individual needs to tube rushed to the hospital or not?-
- Make them sit.
- Ask them to get up and walk 3 metres
- Take a turn.
- Walk 3 metres back and sit down.
While they are performing the test, you need to look out for any peculiar gait, imbalance, feeling of dizziness or unsteadiness.
- Head injury: in a severe head injury, with laceration or contusion, it is very easy to establish that the patient needs to be taken to a hospital. It is in mild to moderate head injuries, that it is important to know whether the individual requires immediate medical assistance and evaluation or not?
In anyone over the age of 60 years, even a very minor/ trivial head injury, it is advised that you go to your doctor. This is important because the presentation of a brain bleed due to an injury/ fall presents differently in the senior age group as compared to a younger patient- which can be ruled out with the help of a smile NCCT Scan.
- Fractures: immobilisation, stabilisation and occasionally surgery are the mainstay of treatment
- Delirium/ acute confusion: a state of mind which is different from the usual, and occurs over a short period of time. When your suspecting delirium, ask the following questions:
- Is there any change in the state of consciousness of the patient?
- Reduced ability to focus?
- Difficulty in understanding the language?
- Any change in the orientation to time, place or person?
- Duration of symptoms?
- Any change in the presentation of the symptoms during the day?
It is important to get a patient with delirium investigated and evaluated, to ascertain the cause. Some common causes that may present as delirium in the elderly are:
- Infection
- Metabolic disturbances/ electrolyte imbalance
- Hypoglycaemia
- Toxic insults, interaction of 2 drugs
- Neurological conditions
- Hypoxia
- Abdominal pain, acidity, heartburn- though common in all age groups, it is more bothersome and concerning in the elderly.
Acute, persistent pain needs to be evaluated in the elderly. Because a serious pathology can present with mild pain as well.
Do not ever ignore abdominal pain, especially if it is acute in nature.
- Heart attack- it can present atypically and might not even present as chest pain. In most, the symptoms seen include- sweating, pain in abdomen, breathlessness- isolated or in adjunct with chest pain.