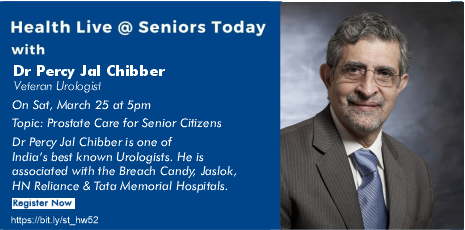
On 25 Mar, 2023, Seniors Today hosted their weekly Health Live Webinar with Dr Percy Jal Chibber, a veteran Urologist who spoke on and answered questions on Prostate Care for Senior Citizens.
Dr Percy Jal Chibber is Senior Consultant Urologist at the Breach Candy and Sir H N Reliance Foundation Hospitals. He is also Director of Urology at the Jaslok Hospital. He has been Honorary Visiting Urological Laparoscopy Specialist to the Tata Memorial Cancer Centre. Although he has been practising in all aspects of urology over the last four decades, his special interests are Endourology, Urologic Laparoscopy, Robotic Surgery and Renal Transplantation.
Dr Percy Jal Chibber took his undergraduate medical education (MBBS) in Mumbai at the B Y L Nair Hospital. He did his postgraduate degree in general surgery (MS) at the same hospital; standing first in the university was awarded four gold medals.
He did his specialist training in Urology at the University of Edinburgh Department of Urology at the Western General Hospital, Edinburgh with the world-renown Professor G D Chisholm and also obtained his fellowship of the Royal College (FRCS). He returned to Mumbai and started his urological practice in 1981, and was soon appointed Honorary Assistant Professor of Urology at the Grant Medical College and the Sir J J Group of Hospitals, where he was later to hold the position of Professor and Head of Urology and Renal Transplantation between 1995 and 2007.
In 1983, Dr Chibber trained in the techniques of Percutaneous Renal Surgery, in UK, and the USA, with Mr J E A Wickham and Dr Arthur Smith, respectively, both of whom have been described as pioneers of Minimally Invasive Urological Surgery.
Since 1983, he has developed and pioneered the techniques of Percutaneous Renal Surgery and Radiology in India, and has one of the largest personal series of the procedure in the world. Since January 2000, he has been performing and training students in the techniques of Laparoscopic Urological Surgery. Dr Chibber was invited by the Cleveland Clinic to spend six weeks as an International Scholar in the department of Laparoscopic Urology in May 2001. He trained in Robotic Urology at the OLV Institute, Alst, Belgium in 2011. He was the President of the Urological Society of India for 2015-2016.
Dr Chibber has published numerous papers in peer-reviewed national and international journals, and has authored chapters in books.
You should get yourself tested for COVID-19, and get an RT-PCR if you have a fever that is persistent for 3 days or more, otherwise there is no need for getting yourself tested, says Dr Chibber on the present surge in the number of covid cases. There is an abundance of viruses that can cause an upper respiratory tract infection, he adds.
The prostate is a walnut shaped gland between the base of the bladder and the apex.
The prostate produces juices that nourish the sperm. The sperm, once it has been ejaculated, forms a coagulum in the vagina and then the juices in the prostate will allow the coagulum to release the sperm and the sperms will travel through the vagina and finally reach the ovum.
When you present to a doctor with urinary complaints, he might put you in a lateral position and put a finger in your anus. Now this is because in the anterior, or the front relationship of the rectum is the prostate. Thus, when the doctor puts his finger in your anus, he can feel your prostate. Digital Rectal Examination is done to determine smoothness, texture, modularity and mucosa of the overlying rectum. It is not done to primarily only determine the size of the prostate.
Functions of Prostate:
- The prostate secretes a slightly alkalic fluid, which is milky in appearance, that usually
constitutes 50-75% of the volume of the semen along with spermatozoa and seminal vesicle fluid.
- Prostate secretion in human consist of proteolytic enzymes, prostatic acid phosphatase, beta-microseminoprotein, prostate- specific antigen and zinc
- The spermatozoa which was expelled in the prostatic fluid have better motility, longer survival and better protection of the genetic material.
- The prostate also contains some smooth muscles that help semen during ejaculation.
Problems of the Prostate:
- Benign Prostate Enlargement: enlargement of the prostate that occurs in every male who has functioning testes. You need testosterone for the prostate to develop as the age advances. Thus, the prostate will enlarge in men after the age of 55 and will be properly enlarged by the age of 65. Everyone between the age group of 55-65 and after will have an enlarged prostate.
- Prostatitis: this is a condition that can occur at all ages but common after middle age. It is caused by the inflammation of the glands in the prostate. It is common in diabetics and other individuals more prone to infections.
- Cancer of prostate: the disease as such has no specific symptoms of its own. But patients with CA prostate will have an enlarged prostate and will thus present with symptoms of an enlarged prostate.
Benign Prostate Enlargement
This is one of the most common enlargements of the prostate.
This is the enlargement of the prostate all men after the age of 55 years develop.
Prostatism
This causes the individual to develop lower urinary tract symptoms such as
- frequency (too often)
- Urgency (too soon)
- Hesitancy (too late)
- Poor emptying (not enough)
- Nocturia (at inconvenient time)
- Dribbling (when they do not want to)
- Retention (cannot pass urine at all)
The cascade that an enlarged prostate causes is as follows:
An enlarged prostate causes an obstruction of the outlet. This leads to poor stream because of the blockage. This leads to an increase in the contraction of the detrusor muscle. The constant contraction of the detrusor muscle makes the bladder thicker, thereby increasing the complaint of frequency, urgency and the urge to urinate at night due to poor contractility. This can also lead to post void residue.
The lower urinary tract symptoms are independent of the prostate size.
USG- KUB when felt necessary is done to ascertain- post void residual urine, bladder wall thickness, presence of stones, dilatation of the upper tracts.
In patients with LUTS we first and foremost rule out CA Prostate.
The second cause that we try to rule out and investigate for is infection. Followed by obstructive bladder pathologies, kidney diseases.
Medical therapy: in 80 % of the patients we are able to control the symptoms and alleviate the complaints, if presented before progression of the disease.
Surgical interventions:
- TURP (Trans Urethral Resection of the Prostate)
- TUIP (Trans Urethral Incision of Prostate)
- TUEvP (Trans Urethral Evaporation of the Prostate)
- HOLEP (Holeium Laser Enucleation of the Prostate)
- GL PVP (GreenLight Phospho-elective Vaporisation of the Prostate)
- RASP (Robot Assisted Simple Prostatectomy)